Maternal deaths in the U.S. spiked in 2021, CDC reports – “There is just no reason for a rich country to have poor maternal mortality”
By Selena Simmons-Duffin and Carmel Wroth
16 March 2023
(NPR) – In 2021, the U.S. had one of the worst rates of maternal mortality in the country’s history, according to a new report from the Centers for Disease Control and Prevention. The report found that 1,205 people died of maternal causes in the U.S. in 2021. That represents a 40% increase from the previous year.
These are deaths that take place during pregnancy or within 42 days following delivery, according to the World Health Organization.
The U.S. rate for 2021 was 32.9 maternal deaths per 100,000 live births, which is more than ten times the estimated rates of some other high income countries, including Australia, Austria, Israel, Japan, and Spain which all hovered between 2 and 3 deaths per 100,000 in 2020.
According to data from the World Health Organization, the maternal mortality rate in high-income nations overall was 12 per 100,000 live births in 2020, while in low-income countries it was 430 per 100,000.
We have to address the social factors that either are barriers to accessing care or that make your medical conditions worse coming into the pregnancy. This is not just about doctors in the hospital.
Dr. Veronica Gillispie-Bell, an OB-GYN at Ochsner Health in Louisiana
International comparisons of maternal deaths are difficult because of differences in methodology in tracking the data, warns the author of the new U.S. report, Donna Hoyert, a health scientist at the National Center for Health Statistics, at the CDC. But, she notes, the U.S. is “usually not faring all that well” on maternal mortality.
“There is just no reason for a rich country to have poor maternal mortality,” says Eileen Crimmins, professor of gerontology at the University of Southern California. The CDC’s latest compilation of data from state committees that review these deaths found that 84% of pregnancy-related deaths in the U.S. were preventable.
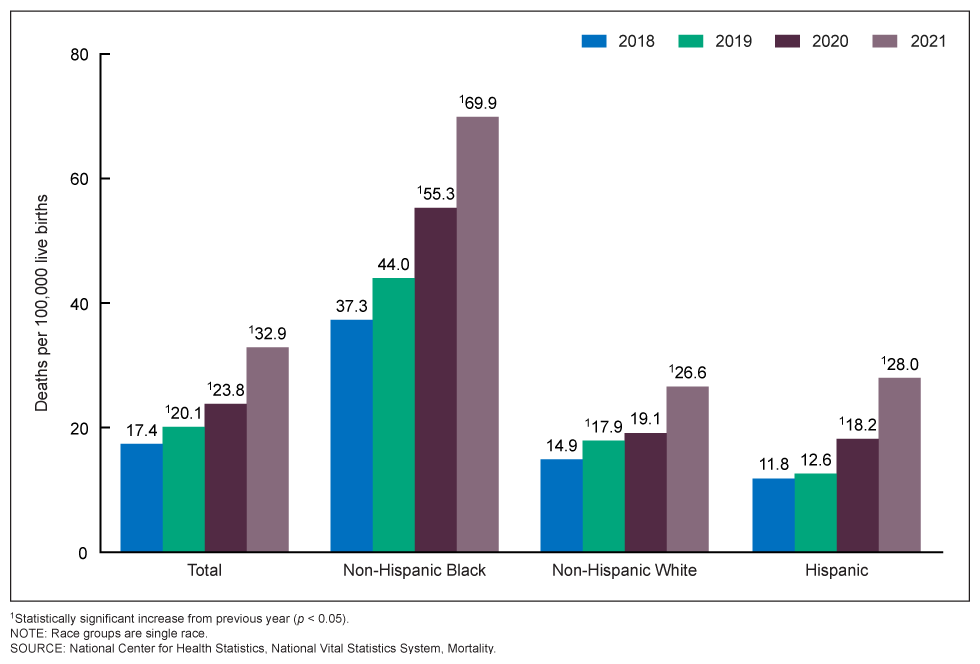
The increase in maternal mortality in 2021 was “seen broadly across different age groups and race and Hispanic-origin groups,” says Hoyert.
She connects the increase in maternal deaths to the COVID-19 pandemic.
“We had some forewarning with the increase between 2019 and 2020 that it looked like maternal mortality rates were increasing during this pandemic period,” she says. “With the overall COVID deaths that occurred in 2021, there was a shift towards younger people, so those would be in the age groups where people would be more likely to be pregnant or recently pregnant.”
She says provisional data suggest the deaths peaked in 2021 and started to go down last year. “So hopefully that’s the apex,” Hoyert says.
Yet some experts worry that other trends around the country could make these figures worse, not better, including abortion restrictions that can delay care for pregnancy complications, and staffing problems at hospitals and closures of rural maternity wards.
The maternal death rate among Black Americans is much higher than other racial groups; in 2021 it was 69.9 per 100,000, which is 2.6 times higher than the rate for White women.
Dr. Veronica Gillispie-Bell, an OB-GYN at Ochsner Health in Louisiana who works with the state’s health department to investigate maternal deaths, says social factors, not biological ones, fuel the racial gap. “We have to address the social factors that either are barriers to accessing care or that make your medical conditions worse coming into the pregnancy,” she says. “This is not just about doctors in the hospital.” [more]
Maternal deaths in the U.S. spiked in 2021, CDC reports
Maternal Mortality Rates in the United States, 2021
By Donna L. Hoyert, Ph.D., Division of Vital Statistics
16 March 2023
(CDC) – This report presents maternal mortality rates for 2021 based on data from the National Vital Statistics System. A maternal death is defined by the World Health Organization as “the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and the site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes” (1). Maternal mortality rates, which are the number of maternal deaths per 100,000 live births, are shown in this report by age group and race and Hispanic origin.
This report updates a previous one that showed maternal mortality rates for 2018–2020 (2). In 2021, 1,205 women died of maternal causes in the United States compared with 861 in 2020 and 754 in 2019 (2). The maternal mortality rate for 2021 was 32.9 deaths per 100,000 live births, compared with a rate of 23.8 in 2020 and 20.1 in 2019 (Table).
In 2021, the maternal mortality rate for non-Hispanic Black (subsequently, Black) women was 69.9 deaths per 100,000 live births, 2.6 times the rate for non-Hispanic White (subsequently, White) women (26.6) (Figure 1 and Table). Rates for Black women were significantly higher than rates for White and Hispanic women. The increases from 2020 to 2021 for all race and Hispanic-origin groups were significant.
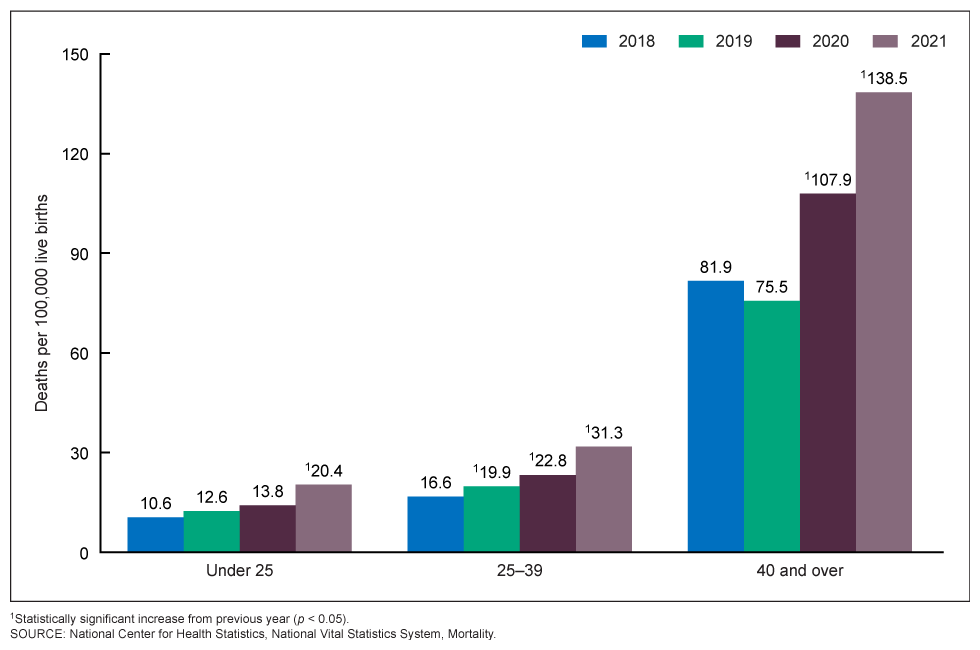
Rates increased with maternal age. Rates in 2021 were 20.4 deaths per 100,000 live births for women under age 25, 31.3 for those aged 25–39, and 138.5 for those aged 40 and over (Figure 2 and Table). The rate for women aged 40 and over was 6.8 times higher than the rate for women under age 25. Differences in the rates between age groups were statistically significant. The increases in the rates between 2020 and 2021 for each of these age groups were statistically significant. [more]