U.S. adult obesity rate tops 40 percent, highest ever recorded – Obesity is single highest risk factor in COVID-19 mortality – “That’s extremely alarming in terms of its medical implications”
18 September 2020 (NBC News) – A new report reveals the adult obesity rate in the United States now stands at more than 42 percent, the highest it’s ever been.
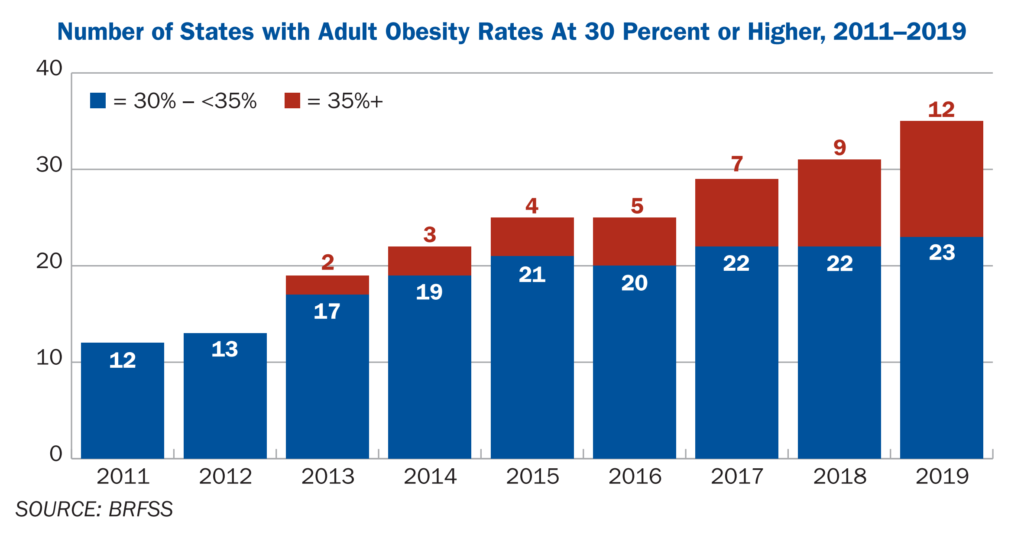
Twelve states have an obesity rate of more than 35 percent.
“That’s extremely alarming in terms of its medical implications,” says John Auerbach, president and CEO of Trust For America’s Health, the group that compiled the report.
Those numbers are also likely still climbing.
The pandemic has plunged millions of families into economic and food insecurity and reduced opportunities for physical activity.
While obesity has long been linked to chronic conditions like diabetes, hypertension and heart disease, emerging evidence also ties it to more severe COVID-19 outcomes, including higher rates in hospitalization and mortality.
“It’s truly life and death now,” Auerbach says. “The number of people who are dying of obesity-related causes has significantly increased with COVID.”
American obesity rates hit record high
The U.S. adult obesity rate tops 40 percent; highest ever recorded. COVID-19 related food insecurity puts more Americans at risk for obesity or worsening obesity.
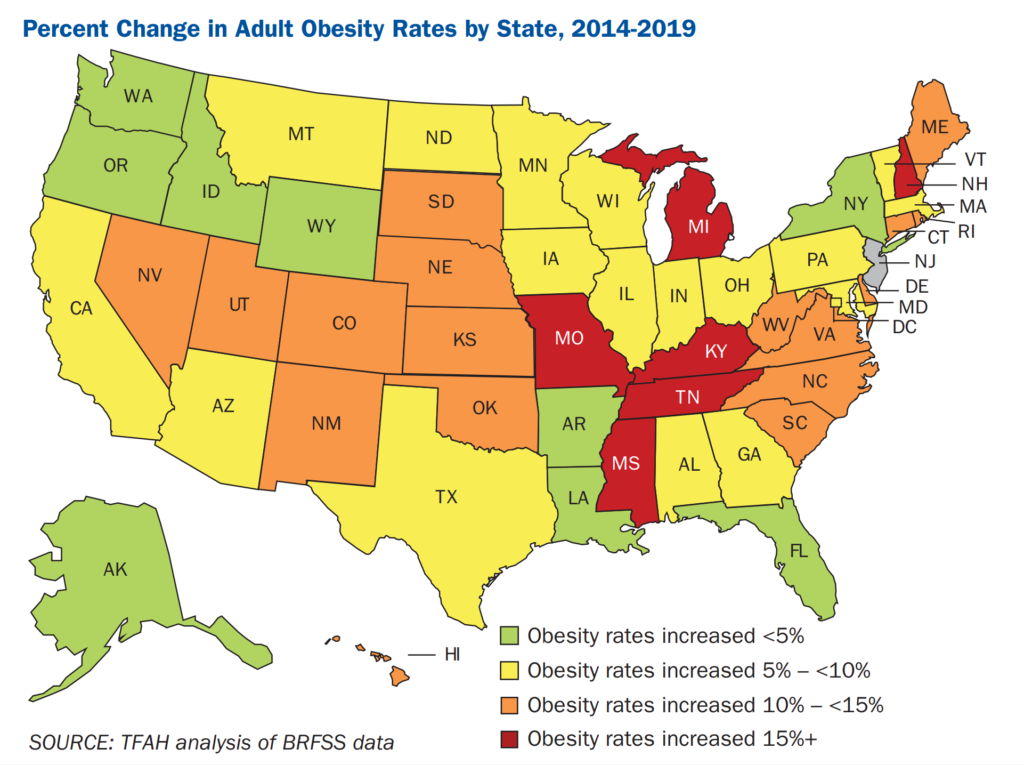
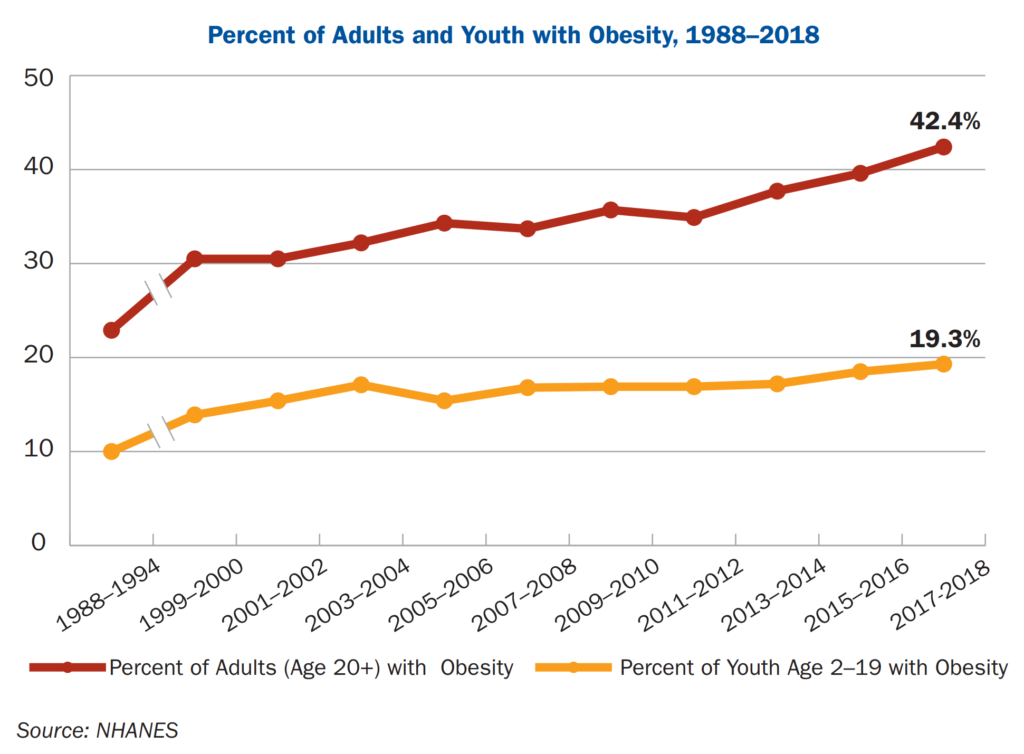
18 September 2020 (Trust for America’s Health) – The U.S. adult obesity rate stands at 42.4 percent, the first time the national rate has passed the 40 percent mark, and further evidence of the country’s obesity crisis. The national adult obesity rate has increased by 26 percent since 2008.
Based in part on newly released 2019 data from the Centers for Disease Control and Prevention’s Behavioral Risk Factors Surveillance System (BFRSS) and analysis by TFAH, this report provides an annual snapshot of rates of overweight and obesity nationwide including by age, gender, race and state of residence [The State of Obesity 2020: Better Policies for a Healthier America pdf].
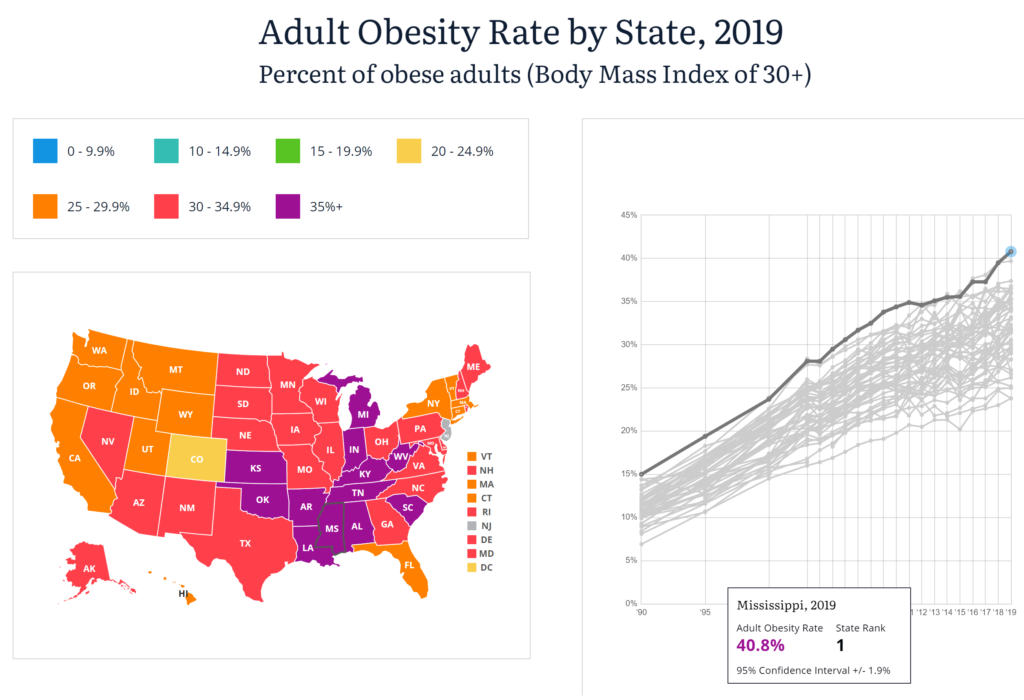
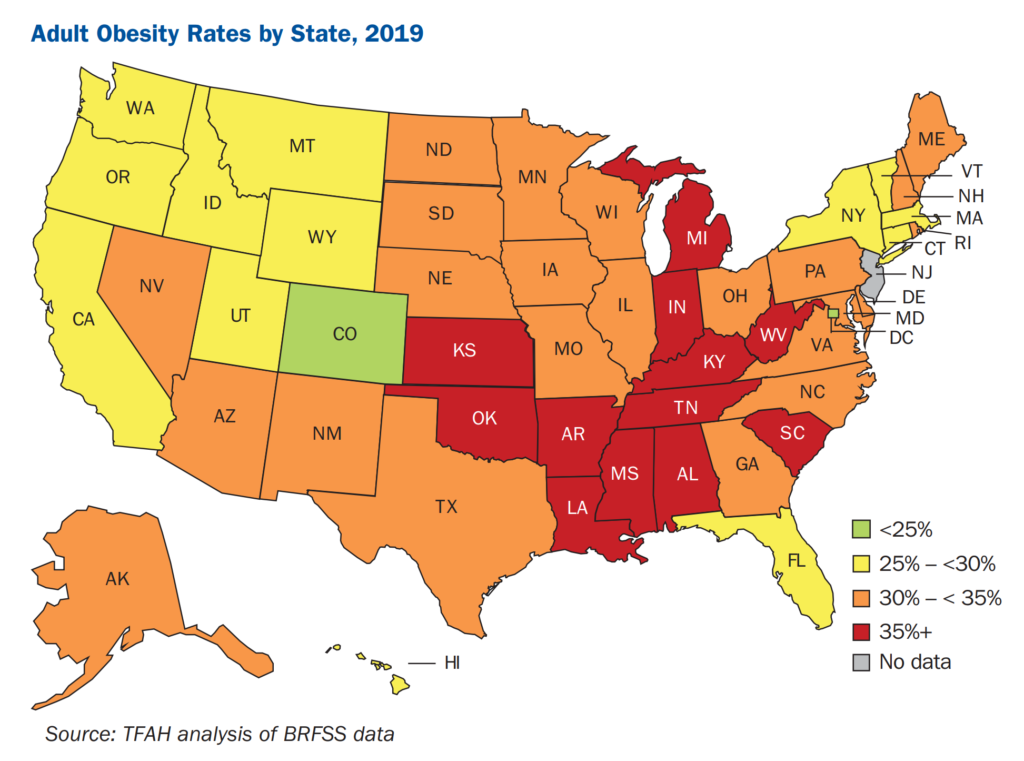
Obesity rates vary considerably between states and regions of the country. Mississippi has the highest adult obesity rate in the country at 40.8 percent and Colorado has the lowest at 23.8 percent. Twelve states have adult rates above 35 percent, they are: Alabama, Arkansas, Indiana, Kansas, Kentucky, Louisiana, Michigan, Mississippi, Oklahoma, South Carolina, Tennessee and West Virginia. As recently as 2012, no state had an adult obesity rate above 35 percent; in 2000 no state had an adult obesity rate above 25 percent.
Rates of childhood obesity are also increasing with the latest data showing that 19.3 percent of U.S. young people, ages 2 to 19, have obesity. In the mid-1970s, 5.5 percent of young people had obesity. Being overweight or having obesity as a young person puts them at higher risk for having obesity and its related health risks as an adult. Furthermore, children are exhibiting earlier onset of what used to be considered adult conditions, including hypertension and high cholesterol.
Demographic trends impact obesity rates
Demographic trends and the conditions in people’s lives have a large impact on their ability to maintain a healthy weight. Generally, the data show that the more a person earns the less likely they are to have obesity. Individuals with less education were also more likely to have obesity. Rural communities have higher rates of obesity and severe obesity than do suburban and metro areas.
Socioeconomic factors such as poverty and discrimination have contributed to higher rates of obesity among certain racial and ethnic populations. Black adults have the highest level of adult obesity nationally at 49.6 percent; that rate is driven in large part by an adult obesity rate among Black women of 56.9 percent. Latinx adults have an obesity rate of 44.8 percent. The obesity rates for white adults is 42.2 percent. Asian adults have an overall 17.4 percent obesity rate.
Obesity and its impact on health including COVID-9 risks
Obesity has serious health consequences including increased risk for type 2 diabetes, high blood pressure, stroke and many types of cancers. Obesity is estimated to increase healthcare spending by $149 billion annually (about half of which is paid for by Medicare and Medicaid) and being overweight or having obesity is the most common reason young adults are ineligible for military service. Concerns about the impact of obesity have taken on new dimensions this year as having obesity is one of the underlying health conditions associated with the most serious consequences of COVID infection, including hospitalization and death. These new data mean that 42 percent of all Americans are at increased risk of serious, possibly fatal, health impacts from COVID-19 due to their weight and health conditions related to obesity.
Food insecurity and its relationship to obesity
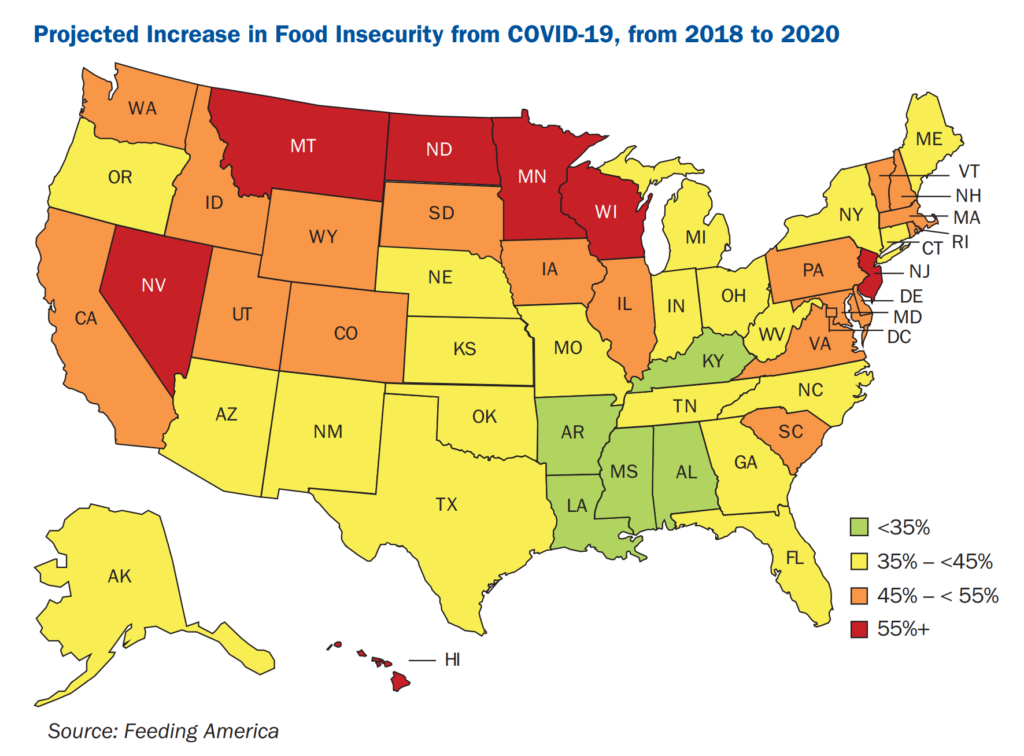
Food insecurity is linked to lower quality diets and tracks with higher levels of obesity in many population groups. Food insecurity is closely linked to economic conditions. There were higher levels of food insecurity during the 2008-2009 financial crisis and early data indicate a large increase in the number of American families experiencing food insecurity due to the COVID-19 crisis. According to U.S. Census Bureau survey data, 25 percent of all respondents and 30 percent of respondents with children, reported experiencing food insecurity between April and June of this year.
Solutions require multi-sector initiatives and policy change
The report includes recommendations on how best to address the obesity crisis grounded in two principles: 1) the need for a multi-sector, multi-disciplinary approach and 2) a focus on those population groups that are disproportionately impacted by the obesity crisis.
Recommendations include:
- While the COVID-19 public health emergency continues to be in place, continue USDA nutrition policy waivers and expand no-cost school meals to all enrolled students for the entire 2020-2021 school year.
- Increase funding to allow for the expansion of critical CDC obesity-prevention programs including the State Physical Activity and Nutrition Program and the Racial and Ethnic Approaches to Community Health program.
- Expand benefits in the Supplemental Nutrition Assistance Program (SNAP, formerly known as “food stamps”) by raising maximum benefit levels, extending Pandemic-EBT (P-EBT) for students and children, doubling investments in SNAP-Ed, and finding innovative, voluntary ways to improve diet quality without harming access or benefit levels.
- Incentivize businesses and public land use to increase access to healthy food options and safe places to be physically active.
- Disincentivize unhealthy food choices by closing tax loopholes and eliminating business-cost deductions related to the advertising of unhealthy food and beverages to children and by enacting sugary drink taxes where tax revenue is allocated to local efforts to reduce health and socioeconomic disparities.
- Encourage Medicaid to cover pediatric weight-management programs for all eligible beneficiaries.
The State of Obesity 2020: Better Policies for a Healthier America
When COVID-19 meets our existing obesity pandemic
By Niran Al-Agba, MD
18 September 2020
(Kitsap Sun) – As of September 2020, nearly 30 million worldwide have tested positive for COVID-19 and it carries a global mortality rate of 3.7%. The largest obstacle to reining in spread of this virus has been the fact that range of symptoms are unpredictable, from minimal to severe respiratory compromise with diffuse lung damage and death. As COVID-19 initially marched across China and Italy, scientists honed in on factors, such as old age, hypertension, diabetes, and coronary artery disease, which placed specific populations at higher risk. Unfortunately, one risk factor has proven to be fairly catastrophic for the United States: Obesity.
The United States has one of the highest rates of obesity in the world. More than 40% of American adults are obese, which means they have a body mass index (BMI) of 30 or higher. Almost 10% of American adults qualify as severely obese, defined as having a BMI of 40 or more. For example, someone who is 5’4” and weighs 235 pounds has a BMI of 40. For reference, normal adults should have a BMI between 18-24.9. Adults are considered overweight with a BMI between 25-29.9. […]

One of the largest studies was published last month in the Annals of Internal Medicine, where researchers examined the records of more than 5000 patients with COVID-19 in the Kaiser Permanente Southern California system. The primary outcome measure of death within 3 weeks of diagnosis. For those with a BMI over 40, the risk of death from COVID-19 was 2.5 times higher and if their BMI was over 45, the risk was 4 times higher.
Those statistics should be somewhat alarming; however, additional findings border on terrifying.
For those patients under 60 years of age, the risk of death increases exponentially with escalating BMI. Compared to their normal weight counterparts, obese patients with a BMI between 35-39.9 are 3 times more likely to die. Of those with extreme obesity — defined as a BMI of 40 or more —the risk of death from COVID-19 is 17 times higher.
As a single risk factor, obesity independently eclipses the mortality risk of other related conditions such as hypertension, diabetes, high cholesterol, or history of a heart attack. Despite the fact that many obese people identify as “healthy,” all bets are off when it comes to fighting COVID-19. [more]