New international report on health care: U.S. suicide rate highest among wealthy nations – U.S. outspends other high-income countries on health care but has lowest life expectancy
30 January 2020 (Commonwealth Fund) – The United States spends substantially more than any other wealthy nation on health care, yet it has a lower life expectancy and a higher suicide rate than its peer nations, according to a new Commonwealth Fund report.
The report, U.S. Health Care from a Global Perspective, 2019: Higher Spending, Worse Outcomes, compares the United States to 10 other high-income nations in the Organization for Economic Cooperation and Development (OECD): Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and the United Kingdom. Commonwealth Fund researchers examined U.S. health care spending, outcomes, risk factors, and quality relative to these other countries. They also compared U.S. performance to the average of all 36 OECD member nations.
Key findings
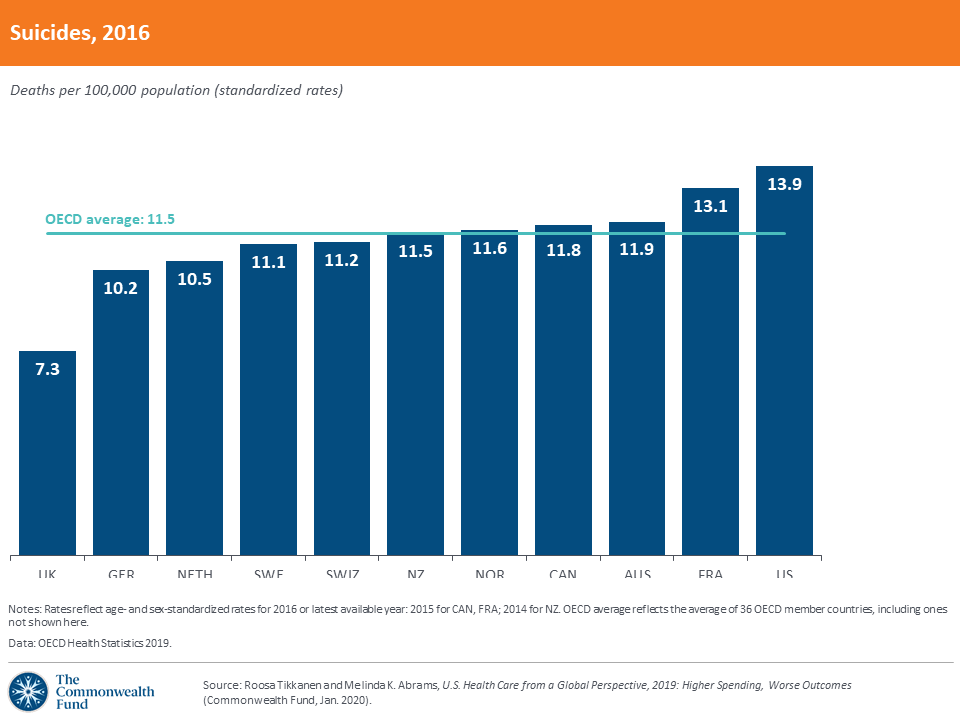
The U.S. has the highest suicide rate of any wealthy nation. Suicides account for 14 deaths per 100,000 people in the U.S. This is double the suicide rate of the United Kingdom. Potential factors that contribute to the high U.S. suicide rate include a high burden of mental illness, a lack of mental health screening, inadequate investment in social services, and the inability of many people to pay for mental health treatment. In recent years, Americans have experienced an uptick in “deaths of despair,” which include suicides and deaths related to substance use and drug overdoses.
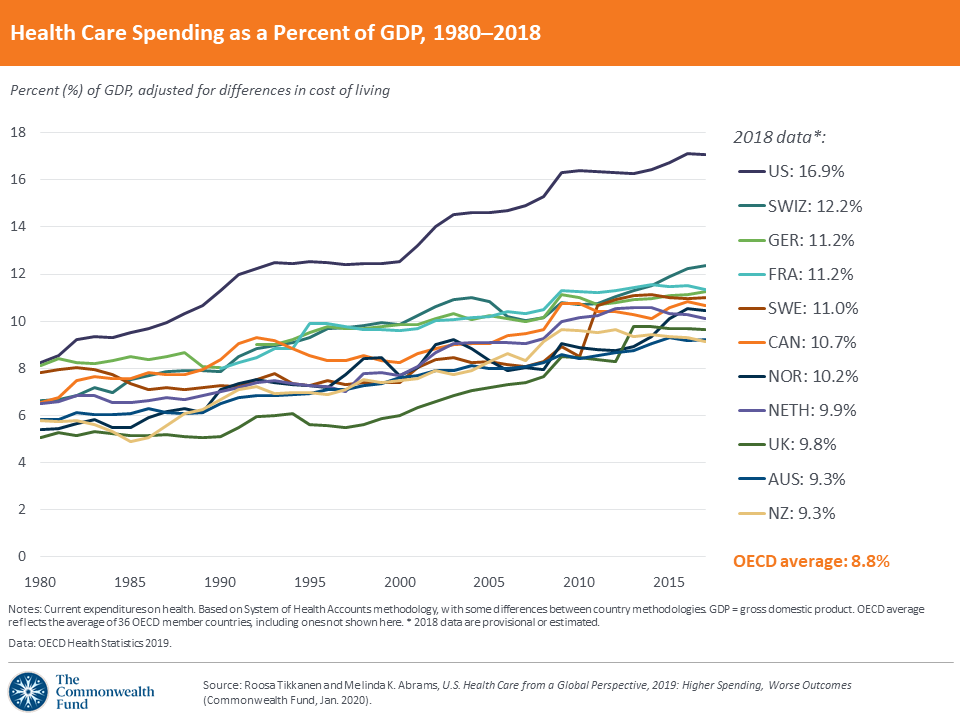
The U.S. spends more on health care than any other high-income country. In 2018, the U.S. spent 16.9 percent of its gross domestic product (GDP) on health care – almost double what the average OECD country spent. In contrast, New Zealand and Australia devoted only 9 percent of GDP to health care. U.S. health spending now totals more than $10,000 per person. Private insurance costs (premiums and employer-sponsored coverage) drive much of this spending in the U.S. The amount of public health care spending in the U.S., meanwhile, is similar to many other countries.
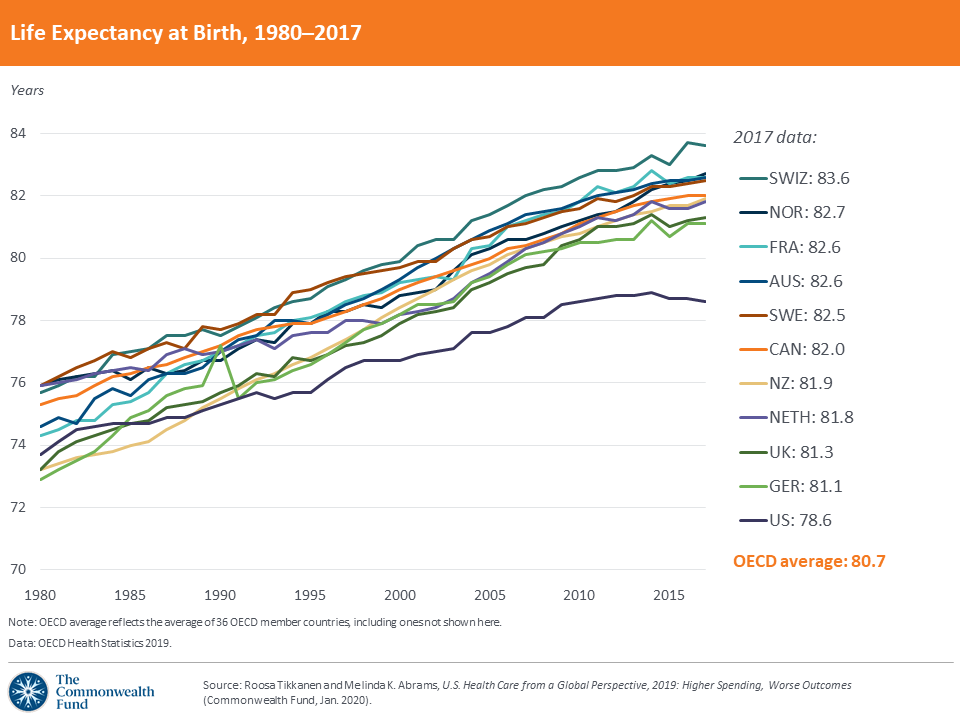
The U.S. has the lowest life expectancy. Despite spending more on health care, Americans have the lowest life expectancy – 78.6 years, a full two years lower than the average for other wealthy nations. People in the U.S. die five years sooner, on average, than people in Switzerland, which has the highest life expectancy in the OECD.
Americans visit the doctor less frequently but use expensive technologies and procedures more often. The average American has only four physician visits per year – approximately half as many as the Dutch and Australians. But the highest rates of MRI scans and hip replacements for older adults are in the U.S.
The U.S. does better than most other high-income nations when it comes to preventive measures such as flu vaccinations and breast cancer screenings. Sixty-eight percent of adults over age 65 in the U.S. had a flu vaccine in 2016, compared to 44 percent in other OECD countries. The U.S. also excels in providing breast cancer screening for women ages 50 to 69, with 80 percent getting appropriate screenings, compared to 61 percent in peer nations, on average. The U.S. fiveyear survival rate for breast cancer is highest among high-income countries — more than five percentage points above the OECD average. However, the U.S. ranks last among the 11 countries on fiveyear survival for cervical cancer, possibly reflecting lower emphasis on screening for this disease.
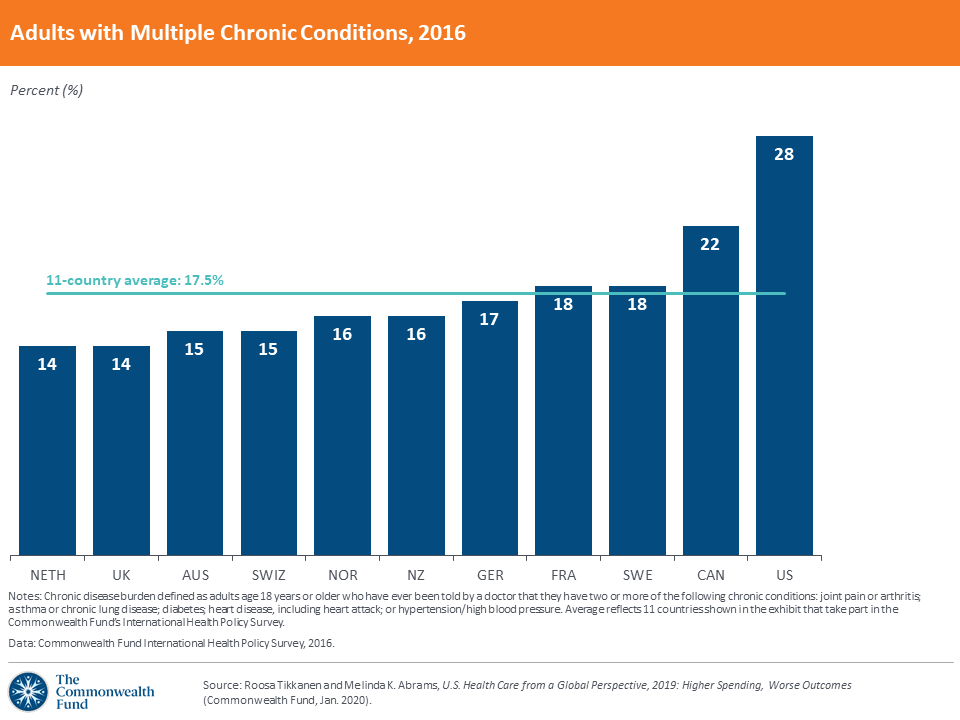
The U.S. has one of the highest rates of hospitalizations for preventable conditions and the highest rate of avoidable deaths. U.S. hospitalizations related to diabetes and hypertension, considered preventable with sufficient access to primary care, are approximately 50 percent higher than the OECD average. Only Germany has a higher rate of preventable hospitalizations for the two conditions. While preventable deaths overall have been falling in each of the 11 nations since 2000, the U.S. continues to have the highest rates of premature deaths from causes such as diabetes, hypertensive diseases, and certain cancers — all considered preventable with timely access to primary care and good chronic disease management.
Implications
The authors recommend some steps to reverse these trends:
- Reduce health care costs. Lowering health care prices is likely to have the greatest impact on U.S. health spending. Other nations take steps to contain costs through budgeting practices and value-based pricing of medical technologies.
- Invest in primary care. Making access to affordable care more readily available and strengthening primary care could make a big difference for the people who need the most care.
- Promote incentives to use effective care and cut down on wasteful care. Recent studies suggest that as much as $935 billion in annual U.S. health care spending goes to ineffective care that provides minimal benefit. The U.S. can learn from other countries and assess what tests and treatments are truly necessary.
How We Conducted This Study
The Commonwealth Fund researchers used data from the OECD’s 2019 health statistics release, which tracks health system measures from 36 high-income countries. The 11 countries included in this comparison take part in the Commonwealth Fund’s annual International Health Policy Survey.
New International Report on Health Care: U.S. Suicide Rate Highest Among Wealthy Nations