U.S. depression rates reach new highs in 2023
By Dan Witters
17 May 2023
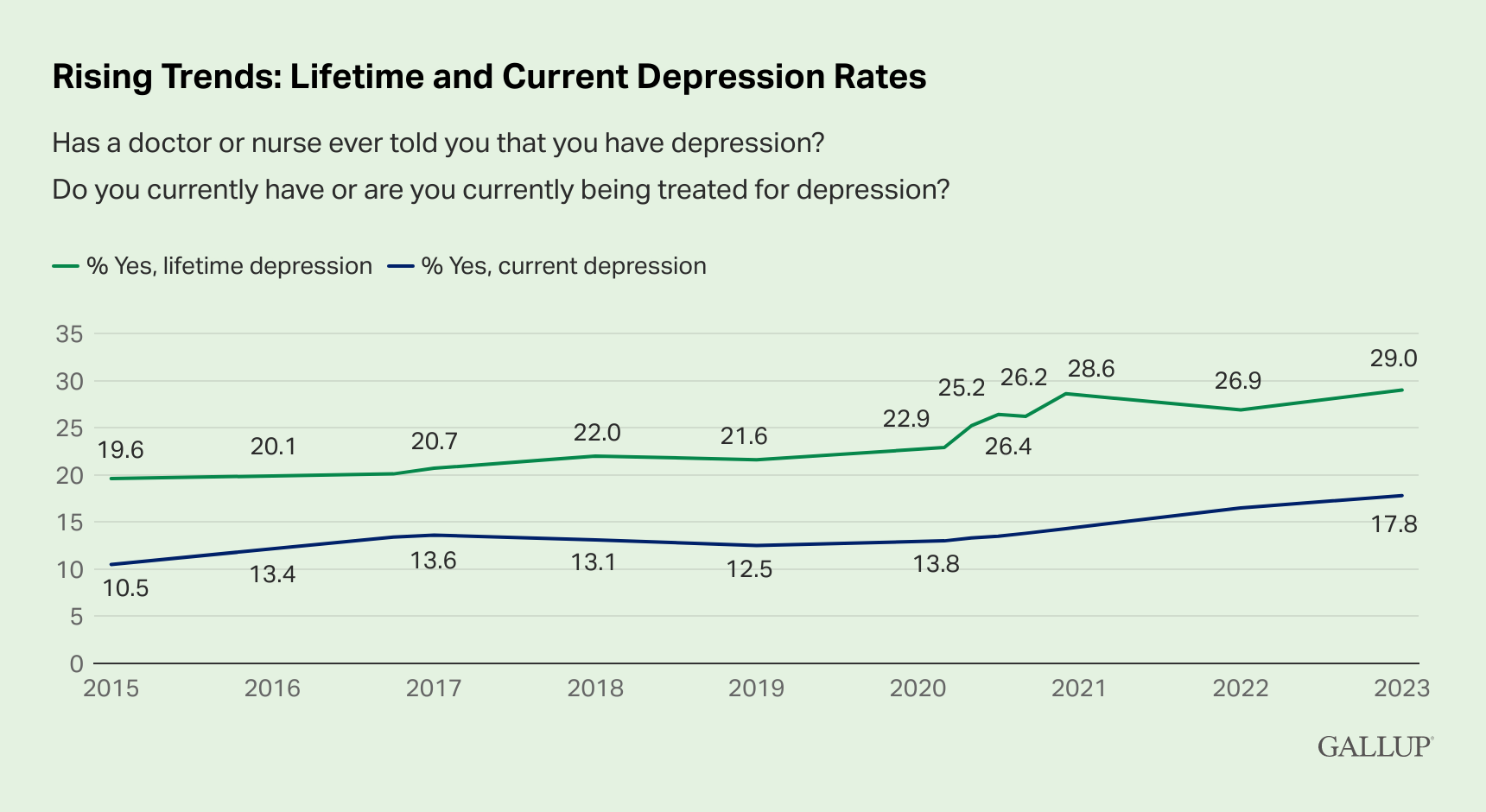
WASHINGTON, D.C. (Gallup) – The percentage of U.S. adults who report having been diagnosed with depression at some point in their lifetime has reached 29.0%, nearly 10 percentage points higher than in 2015. The percentage of Americans who currently have or are being treated for depression has also increased, to 17.8%, up about seven points over the same period. Both rates are the highest recorded by Gallup since it began measuring depression using the current form of data collection in 2015.
The most recent results, obtained Feb. 21-28, 2023, are based on 5,167 U.S. adults surveyed by web as part of the Gallup Panel, a probability-based panel of about 100,000 adults across all 50 states and the District of Columbia. Respondents were asked, “Has a doctor or nurse ever told you that you have depression?” and “Do you currently have or are you currently being treated for depression?” Both metrics are part of the ongoing Gallup National Health and Well-Being Index.
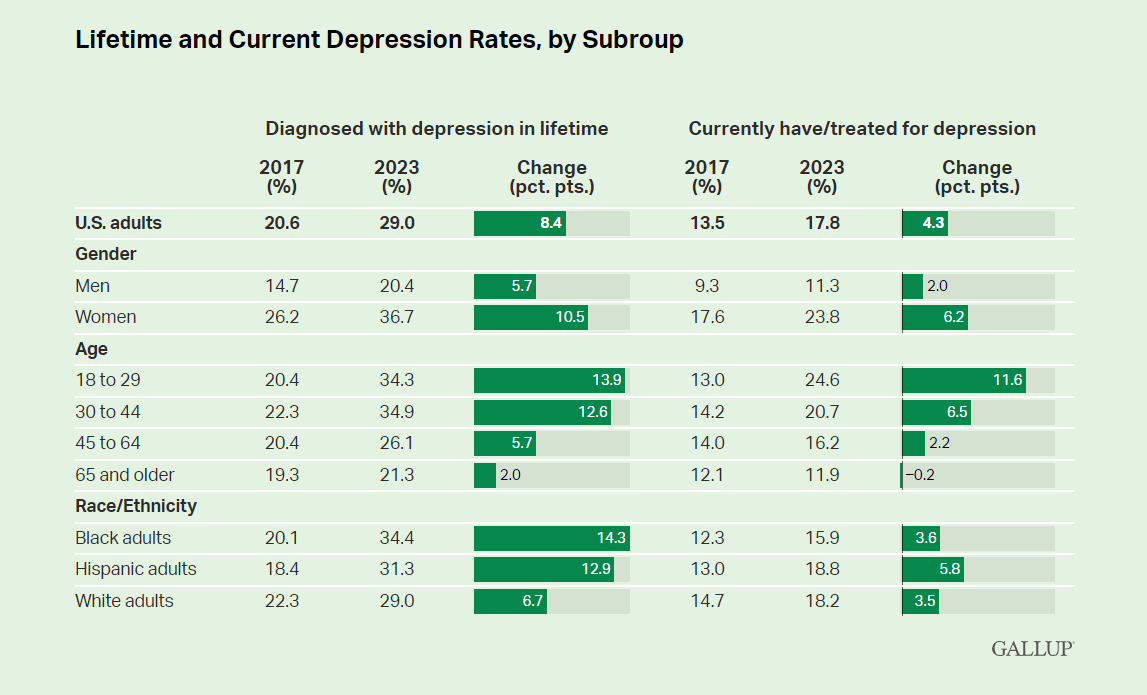
Rates Among Women, Young Adults, Black and Hispanic Adults Rising Fastest
Over one-third of women (36.7%) now report having been diagnosed with depression at some point in their lifetime, compared with 20.4% of men, and their rate has risen at nearly twice the rate of men since 2017. Those aged 18 to 29 (34.3%) and 30 to 44 (34.9%) have significantly greater depression diagnosis rates in their lifetime than those older than 44.
Women (23.8%) and adults aged 18 to 29 (24.6%) also have the highest rates of current depression or treatment for depression. These two groups (up 6.2 and 11.6 percentage points, respectively), as well as adults aged 30 to 44, have the fastest-rising rates compared with 2017 estimates.
Lifetime depression rates are also climbing fast among Black and Hispanic adults and have now surpassed those of White respondents. (Historically, White adults have reported marginally higher rates of both lifetime and current depression.)
Implications
Alarming rates of depression are not unique to the U.S. Globally, nearly four in 10 adults aged 15 and older either endure significant depression or anxiety themselves or have a close friend or family member who suffers from it. Other Gallup research has estimated that 22% of Northern American adults have experienced depression or anxiety so extreme that they could not continue regular daily activities for two weeks or longer, similar to a global rate of 19% and matching estimates found in Western Europe, the Middle East and North Africa, and South Asia.
Clinical depression had been slowly rising in the U.S. prior to the COVID-19 pandemic but has jumped notably in its wake. Social isolation, loneliness, fear of infection, psychological exhaustion (particularly among front-line responders such as healthcare workers), elevated substance abuse and disruptions in mental health services have all likely played a role. While experiences of significant daily loneliness have subsided in the past two years amid widespread vaccinations and a slow return to normalcy, elevated loneliness experiences during the pandemic likely played a substantive role in increasing the rates of the longer-term, chronic nature of depression. Currently, 17% of U.S. adults report experiencing significant loneliness “yesterday,” projecting to an estimated 44 million people.
Among subgroups, women have historically reported substantially higher levels of depression than men. That this gap has notably widened further since 2017 is likely explained by several COVID-related factors, including the fact that women were disproportionately likely to lose their jobs or to exit the workforce altogether due in part to the pandemic driving children home from school or day care. Women also made up 78% of workers in all healthcare occupations in 2019, exposing them to enhanced emotional and psychological risk associated with the pandemic.
Young adults, in turn, are more likely to be single and to report loneliness, particularly so during the pandemic. They also need more social time to boost their mood than older adults, something directly impacted by COVID-19. Daily experiences of sadness, worry and anger — all of which are closely related to depression — are highest for those under 30 and those with lower income levels. And, like women, young adults and people of color were disproportionately likely to lose their jobs altogether due to the pandemic.