The U.S. maternal health divide: The limited maternal health services and worse outcomes of states proposing new abortion restrictions
By Eugene Declercq, Ruby Barnard-Mayers, Laurie Zephyrin, and Kay Johnson
14 December 2022
(Commonwealth Fund) – In anticipation of a U.S. Supreme Court decision overturning Roe v. Wade, a number of states passed “trigger laws” that would ban all, or nearly all, abortions once national abortion protections ended. In the months since the Court’s ruling in Dobbs v. Jackson Women’s Health Organization in June 2022, several of these states have in fact banned abortion in most instances.1 Other states have enacted bans or severe restrictions since then, and others may do so in the coming months or years.2
In this brief, we assess the current state of maternal and infant health in these states, identify weaknesses in perinatal care systems, and consider how abortion bans may exacerbate these weaknesses. We compare states that have current or proposed abortion bans or restrictions with states that are unlikely to pass such restrictions, focusing on the following areas:
- the availability of maternal care resources such as maternity care providers
- maternal and infant health status and outcomes
- health coverage policies related to accessing maternity care
- performance of the health system in providing equitable access and care.
For our analysis, we compared health status and health care resources in the 26 states that the Guttmacher Institute has identified as having “restrictive,” “very restrictive,” or “most restrictive” policies on abortion — which we refer to as “abortion-restriction states” — to those in the 24 “abortion-access states” that, along with the District of Columbia, have not instituted bans or new restrictions on abortion.3 […]
Differences in Maternity Care Resources
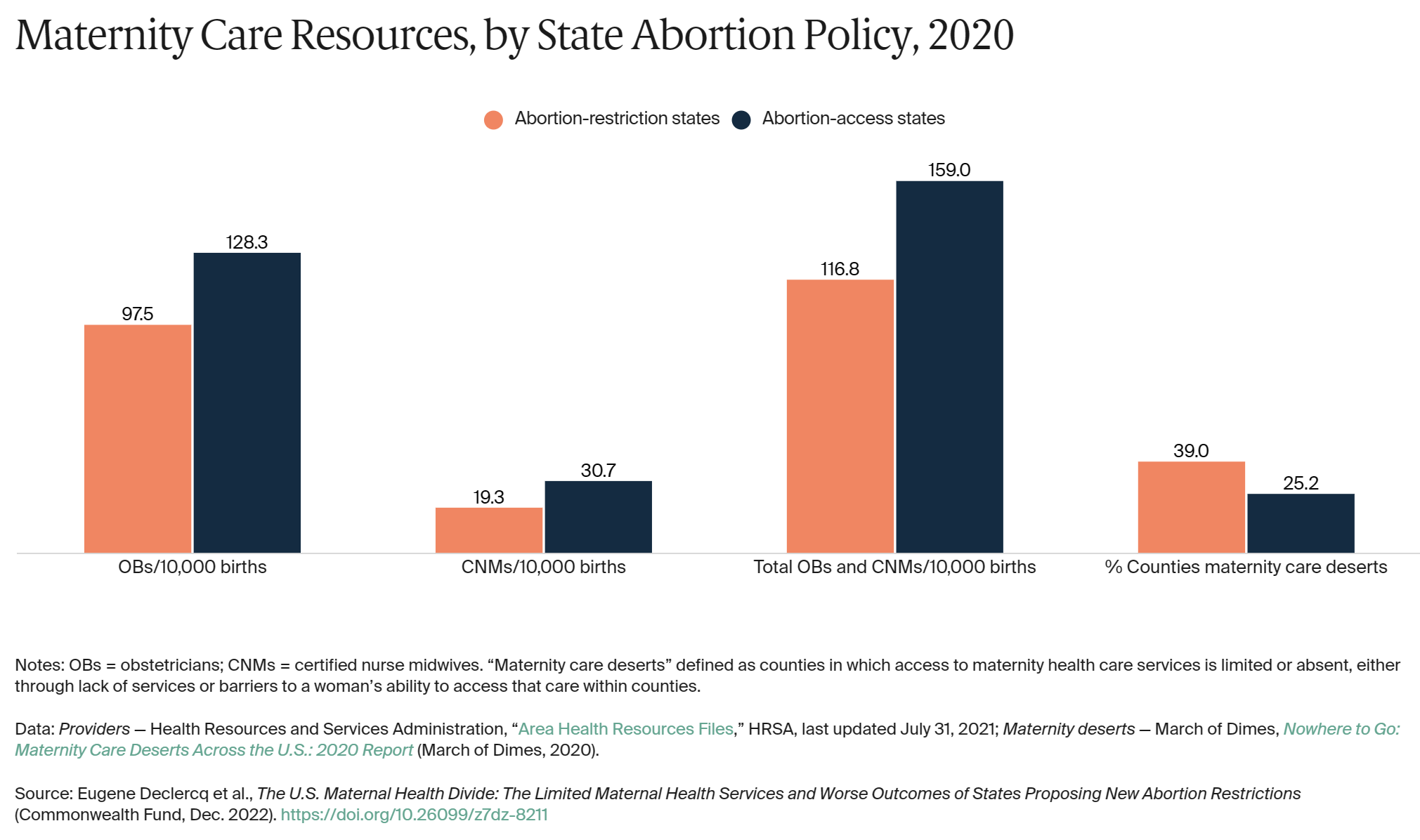
In mapping the availability of maternity care resources, including obstetric care, birth centers, ob/gyns, and certified nurse midwives, across the United States, the March of Dimes uncovered a large number of maternity care “deserts” — defined as counties in which access to maternity health care services is limited or absent, either through lack of services or barriers to a woman’s ability to access that care within counties.4 Our analysis shows that 39 percent of counties in abortion-restriction states can be considered maternity care deserts, compared with 25 percent of counties in abortion-access states. This disparity may be partially explained by the greater number of births in abortion-restriction states that occur in rural areas, where access to maternity care is more limited and maternity care deserts are more common. Rural areas account for 17 percent of births in abortion-restriction states, but only 8 percent in abortion-access states (data not shown).
As Exhibit 3 shows, abortion-restriction states also have fewer maternal care providers than states with abortion access, including a 32 percent lower ratio of obstetricians to births and a 59 percent lower ratio of certified nurse midwives to births. After the Dobbs decision, this disparity could worsen, as some maternity care providers have been reported to be reluctant to work in states where they might face legal challenges to their practice.5
The lack of maternity resources could mean not only more limited access to birthing services but also greater difficulty for pregnant people in accessing early and continuous prenatal care.6 In abortion-restriction states in 2020, the proportion of individuals giving birth who had no prenatal care or late prenatal care was 62 percent greater than for someone giving birth in abortion-access states (7.3% vs. 4.5%; data not shown).
Differences in Maternal Health Outcomes
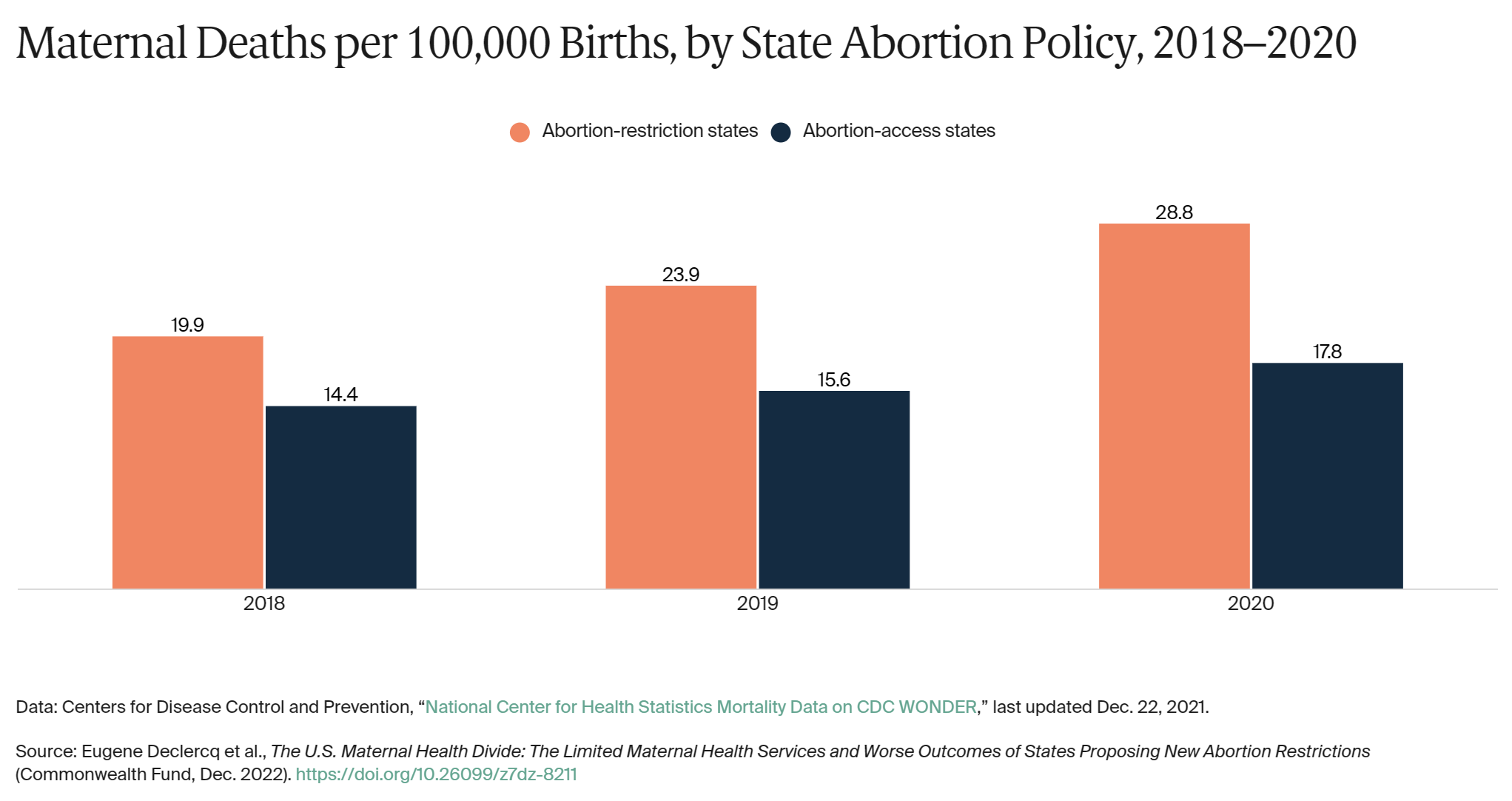
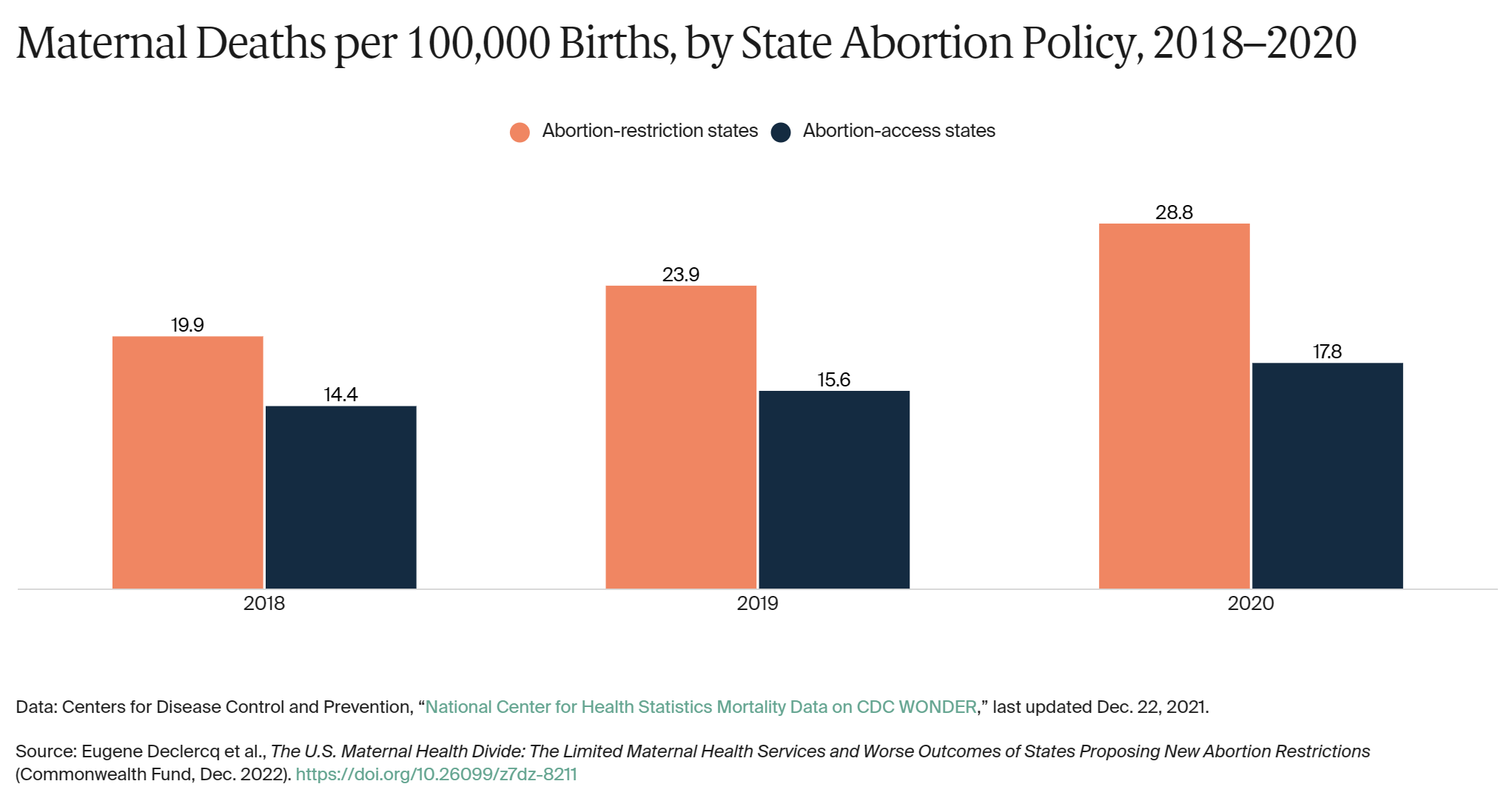
To compare maternal death rates (deaths during pregnancy, at birth, or within 42 days of birth) in states with abortion bans or restrictions to those without, we examined the most recent three years of data.7 We found that maternal death rates were 62 percent higher in 2020 in abortion-restriction states than in abortion-access states (28.8 vs. 17.8 per 100,000 births). Notably, across the three years presented in Exhibit 4, the maternal mortality rate was increasing nearly twice as fast in states with abortion restrictions.
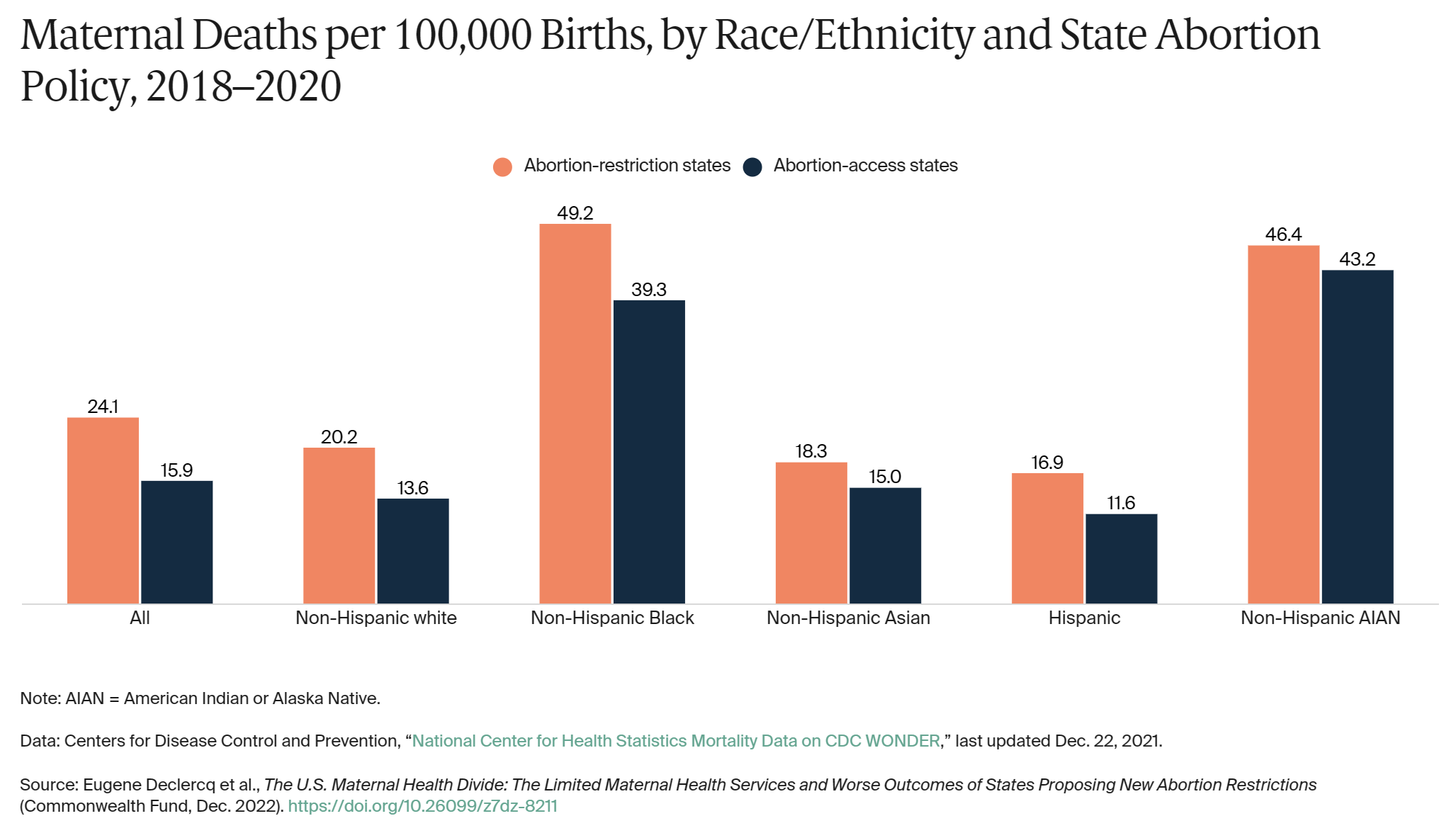
Maternal deaths are high in the U.S. relative to other high-income countries, and there are significant inequities by race and ethnicity.8 In addition, for every major racial or ethnic group, maternal death rates are higher in abortion-restriction states compared to abortion-access states, including 20 percent higher among non-Hispanic Black people, 33 percent higher among non-Hispanic white people, and 31 percent higher among Hispanic people (Exhibit 5).
The differences among states are not limited to pregnancy-related deaths. As shown in Exhibit 6, overall death rates for women of reproductive age (15–44) in abortion-restriction states were 34 percent higher than in abortion-access states (104.5 vs. 77.9 per 100,000 people).
Differences in Perinatal Health Outcomes
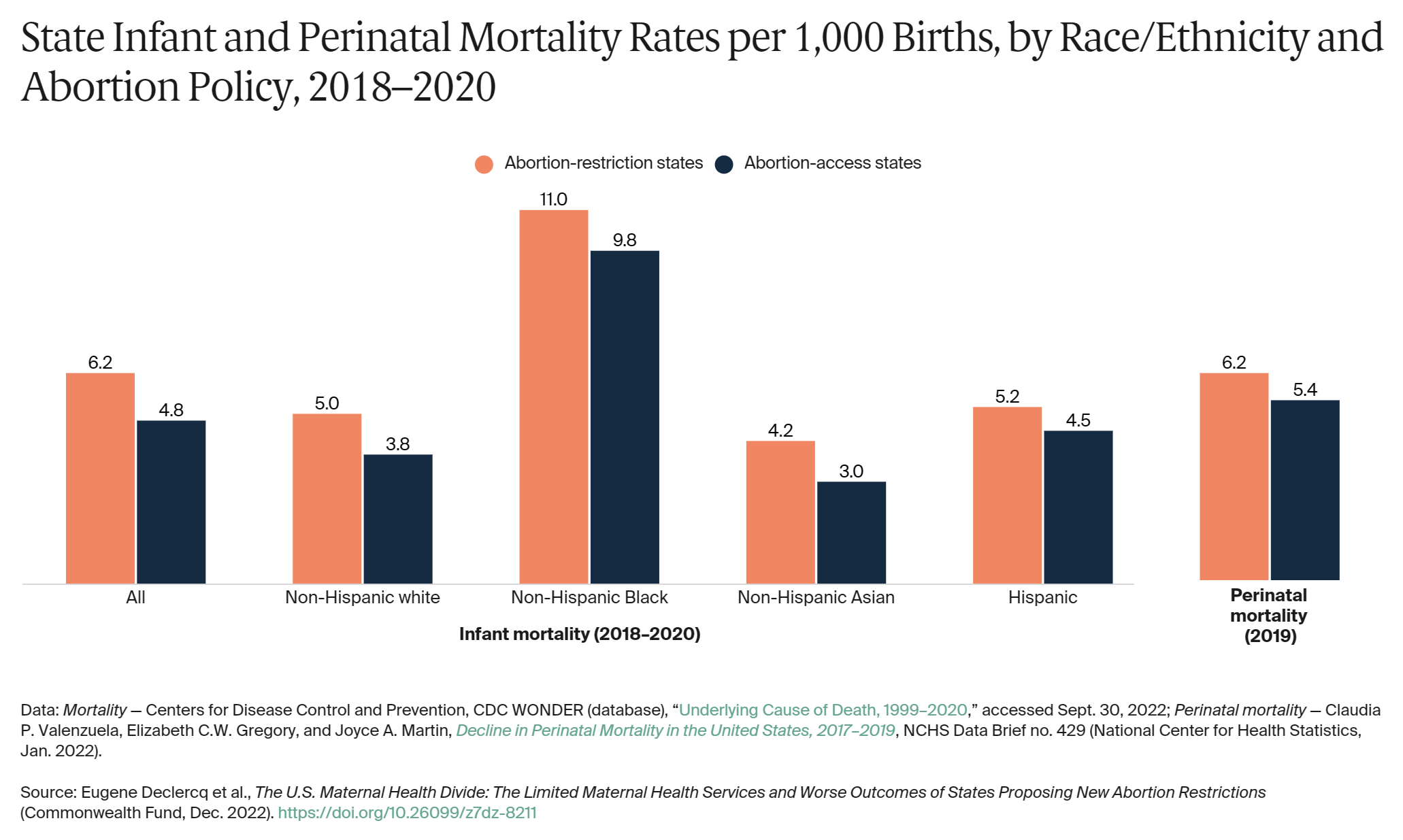
Perinatal outcomes are also worse in states with abortion bans or restrictions: in 2019, perinatal deaths (fetal deaths or infant deaths in the first week of life) occurred at a 15 percent higher rate, on average, than in states with abortion access (Exhibit 7).9
States with abortion bans or restrictions also had higher neonatal death rates in the first 27 days of life (4.05 deaths vs. 3.23 deaths per 1,000 births), as well as higher postneonatal mortality rates between 28 and 365 days after birth (2.16 deaths vs. 1.54 deaths per 1,000 births; data not shown).
Mortality in the first year of life among non-Hispanic Black infants was at least double that of other groups in both abortion-restriction and abortion-access states. In all cases, infant mortality was higher in abortion-restriction states: 41 percent higher for non-Hispanic Asian infants, 34 percent higher for non-Hispanic white infants, and 12 percent higher for non-Hispanic Black infants.
Differences in Equity
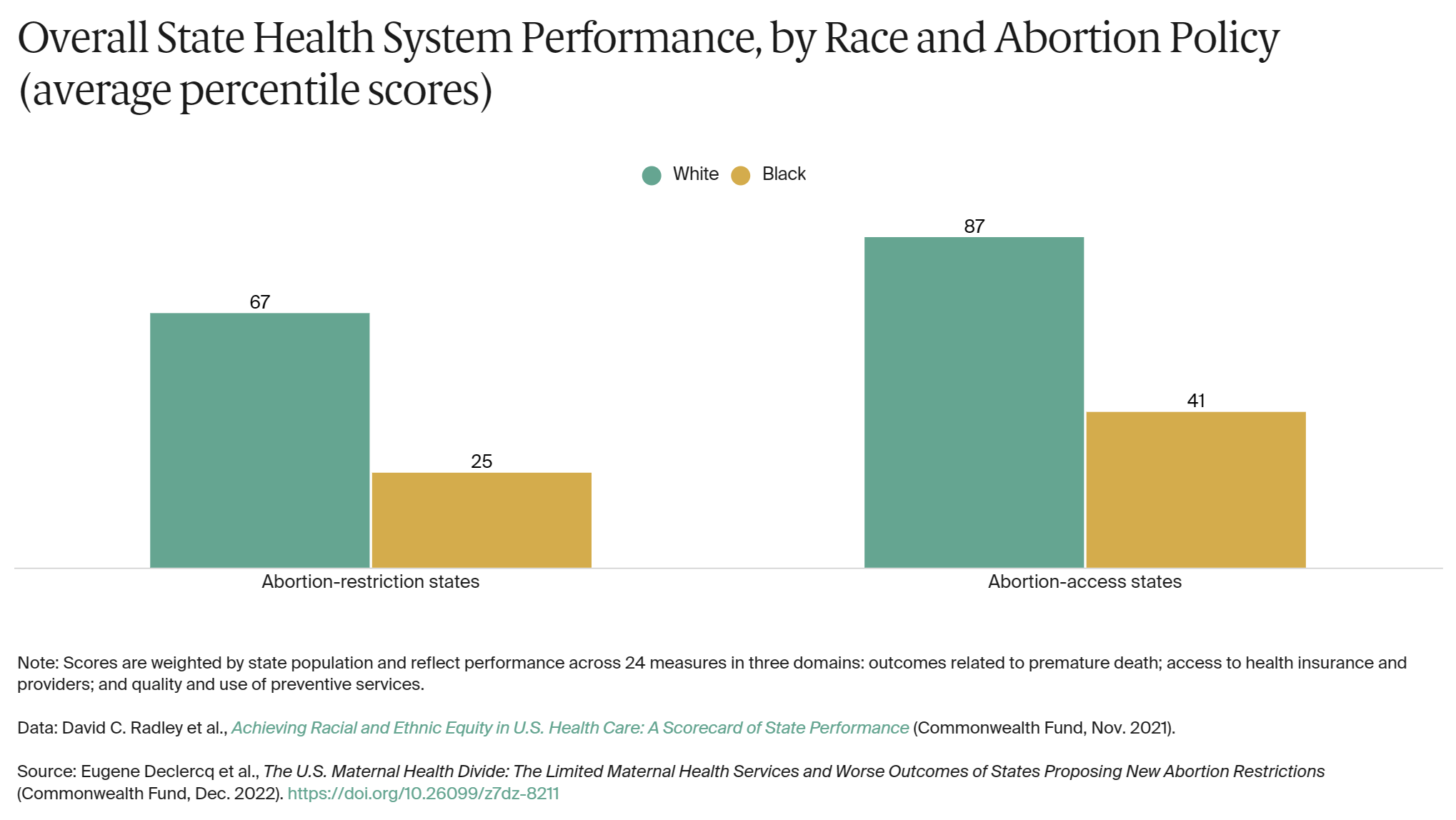
We also compared states with and without abortion bans or restrictions based on the Commonwealth Fund’s health equity scorecard, a national dataset that assesses how state health care systems in the U.S. are functioning for people of color.10 Each state’s score is based on 24 health system performance indicators across the following three domains: 1) outcomes related to premature death (for example, breast cancer deaths); 2) access to health insurance and health care providers (such as adults age 18 and older who have a usual source of care); and 3) quality and use of preventive care services (such as adults age 18 and older who received a flu shot in the past year).
The scores in Exhibit 8 are average percentile scores on overall performance across the three domains (a higher score reflects greater equity). Abortion-access states perform better overall for both white and Black people than abortion-restriction states do. […]
Conclusion
Compared with their counterparts in other states, women of reproductive age and birthing people in states with current or proposed abortion bans have more limited access to affordable health insurance coverage, worse health outcomes, and lower access to maternity care providers. Making abortion illegal risks widening these disparities, as states with already limited Medicaid maternity coverage and fewer maternity care resources lose providers who are reluctant to practice in states that they perceive as restricting their practice.15 The result is a deepening of fractures in the maternal health system and a compounding of inequities by race, ethnicity, and geography.
States have it within their power to avoid that outcome. In partnership with health plans, providers, and residents, state leaders could attempt to recruit more maternity care providers — including midwives, physicians, doulas, and nurses — and promote the operation of more birthing facilities, such as hospital units and birthing centers. Additional support could be provided to community-based organizations and to perinatal health care teams, through a combination of Medicaid and public health funding, and provider financial incentives could drive better quality in maternal health care. And by adopting the Affordable Care Act’s Medicaid eligibility expansion for low-income adults and extending Medicaid postpartum coverage to one year, states could enhance the health and well-being of mothers and infants before, during, and beyond pregnancy.
Increased federal funding for reproductive health care, family planning, maternity care, and care delivery system transformations also could mitigate the impact of the Dobbs decision and state abortion bans on people’s lives. State, congressional, and executive branch actions are all needed to protect the health of women and birthing people and ensure optimal and equitable outcomes for mothers and infants.
How We Conducted This Study
We drew our data from a wide range of sources, which are noted in the respective exhibits and the appendix. These include national birth and death data from CDC WONDER, the classification of states with maternity care deserts from the March of Dimes, health workforce data from the Area Health Resources Files, and state equity outcomes from the Commonwealth Fund report Achieving Racial and Ethnic Equity in U.S. Health Care: A Scorecard of State Performance.16 The organizations producing the original data were not responsible for this secondary data analysis.
Whenever possible, the most recent data available were used. In some cases where data at the state level may involve smaller numbers (such as maternal deaths), years were combined to provide more stable estimates.
We recognize there’s no definitive characterization of which states will be passing abortion bans in the next few months. In this analysis, we have used the Guttmacher Institute classifications of “restrictive,” “very restrictive,” or “most restrictive” to identify states with abortion restrictions as of 15 November 2022. We understand these classifications can shift over time, but the general pattern of differences has remained consistent. We also recognize that in some states listed as nonrestrictive, certain restrictions exist, but these are balanced by some protections as well. [more]
NOTES
- Sara Rosenbaum, Katie Keith, and Timothy S. Jost, “The United States Supreme Court Ends the Constitutional Right to Abortion,” To the Point (blog), Commonwealth Fund, June 27, 2022.
- Guttmacher Institute, “Interactive Map: U.S. Abortion Policies and Access After Roe,” updated as of Nov. 15, 2022.
- Guttamacher Institute, “Interactive Map,” 2022.
- March of Dimes, Nowhere to Go: Maternity Care Deserts Throughout the U.S.: 2020 Report (March of Dimes, 2020).
- American Society for Reproductive Medicine, States’ Abortion Laws: Potential Implications for Reproductive Medicine (ASRM, Oct. 2022).
- Peter Shin et al., In the Wake of Dobbs, Are Community Health Centers Prepared to Respond to Rising Maternal and Infant Care Needs? (George Washington University, July 2022).
- For a discussion of maternal mortality rates, see Eugene Declercq and Laurie Zephyrin, Maternal Mortality in the United States: A Primer (Commonwealth Fund, Dec. 2020).
- Donna L. Hoyert, Maternal Mortality Rates in the United States, 2020 (National Center for Health Statistics, Feb. 2022).
- Claudia P. Valenzuela, Elizabeth C.W. Gregory, and Joyce A. Martin, Decline in Perinatal Mortality in the United States, 2017–2019, NCHS Data Brief no. 429 (National Center for Health Statistics, Jan. 2022).
- David C. Radley et al., Achieving Racial and Ethnic Equity in U.S. Health Care: A Scorecard of State Performance (Commonwealth Fund, Nov. 2021).
- Office of the Assistant Secretary for Planning and Evaluation, “2022 Poverty Guidelines,” U.S. Department of Health and Human Services, n.d.
- Peter Shin et al., “What Are Talevski’s Implications for Community Health Centers and Their Patients? Estimating the Impact of Losing Federally Enforceable Medicaid FQHC Payment Rights,” GW Health Policy & Management Matters, George Washington University, Sept. 14, 2022.
- Henry J. Kaiser Family Foundation, “Medicaid Postpartum Coverage Extension Tracker,” accessed Oct. 20, 2022.
- Jamila Michener, A Racial Equity Framework for Assessing Health Policy (Commonwealth Fund, Jan. 2022).
- ASRM, States’ Abortion Laws, 2022.
- Radley et al., Achieving Racial and Ethnic Equity, 2021.