U.S. excess deaths rose a staggering 23 percent in 2020 – “They said they were opening early to rescue the economy. The tragedy is that not only cost more lives but actually hurt their economy by extending the length of the pandemic.”
By Mary Kate Brogan
2 April 2021
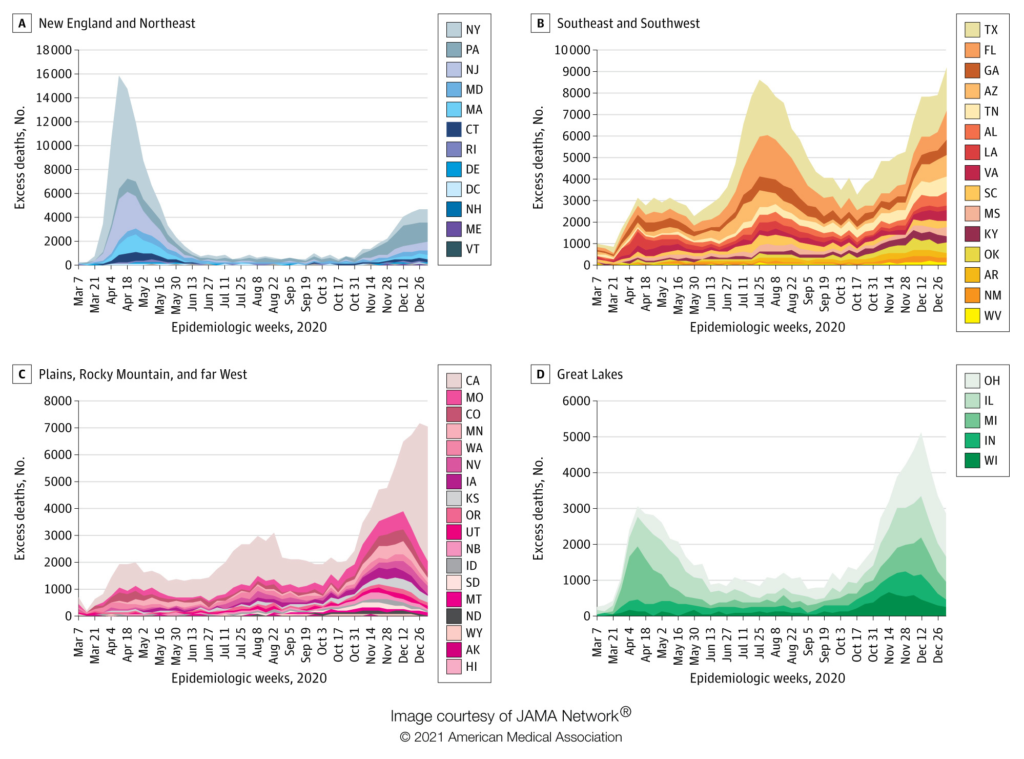
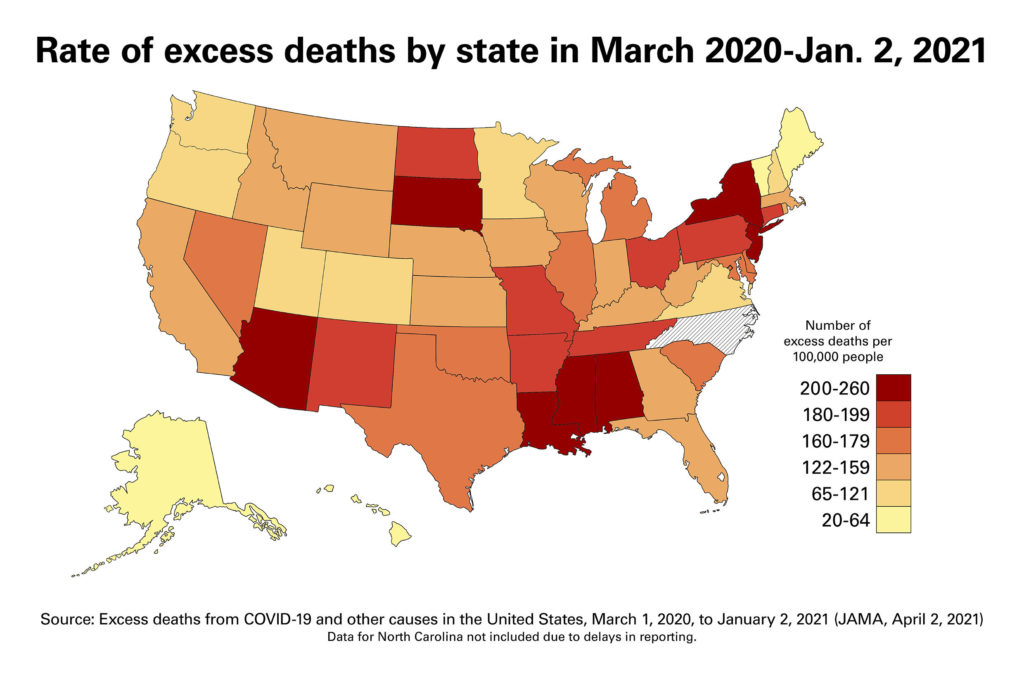
(VCU News) – Extended surges in the South and West in the summer and early winter of 2020 resulted in regional increases in excess death rates, both from COVID-19 and from other causes, a 50-state analysis of excess death trends has found. Virginia Commonwealth University researchers’ latest study notes that Black Americans had the highest excess death rates per capita of any racial or ethnic group in 2020.
The research, published Friday in the Journal of the American Medical Association, offers new data from the last 10 months of 2020 on how many Americans died during 2020 as a result of the effects of the pandemic — beyond the number of COVID-19 deaths alone — and which states and racial groups were hit hardest.
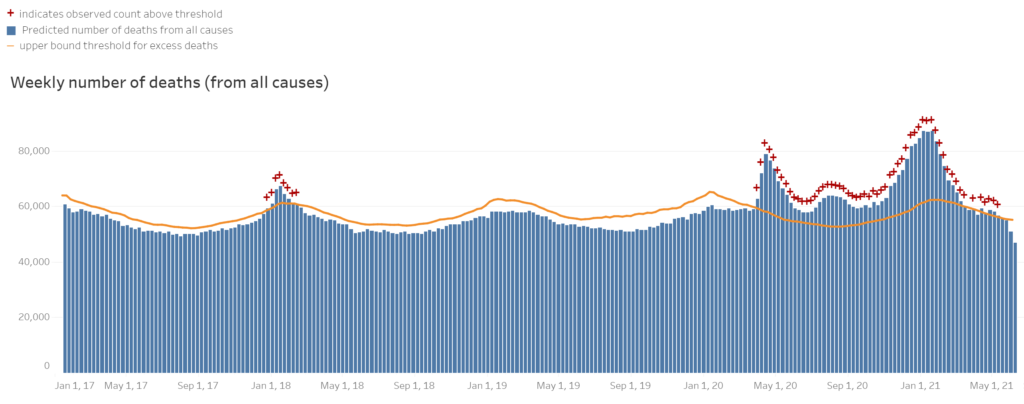
The rate of excess deaths — or deaths above the number that would be expected based on averages from the previous five years — is usually consistent, fluctuating 1% to 2% from year to year, said Steven Woolf, M.D., the study’s lead author and director emeritus of VCU’s Center on Society and Health. From March 1, 2020, to Jan. 2, 2021, excess deaths rose a staggering 22.9% nationally, fueled by COVID-19 and deaths from other causes, with regions experiencing surges at different times.
They said they were opening early to rescue the economy. The tragedy is that policy not only cost more lives, but actually hurt their economy by extending the length of the pandemic. One of the big lessons our nation must learn from COVID-19 is that our health and our economy are tied together. You can’t really rescue one without the other.
Steven Woolf, M.D., director emeritus of VCU’s Center on Society and Health
“COVID-19 accounted for roughly 72% of the excess deaths we’re calculating, and that’s similar to what our earlier studies showed. There is a sizable gap between the number of publicly reported COVID-19 deaths and the sum total of excess deaths the country has actually experienced,” Woolf said.
For the other 28% of the nation’s 522,368 excess deaths during that period, some may actually have been from COVID-19, even if the virus was not listed on the death certificates due to reporting issues.
But Woolf said disruptions caused by the pandemic were another cause of the 28% of excess deaths not attributed to COVID-19. Examples might include deaths resulting from not seeking or finding adequate care in an emergency such as a heart attack, experiencing fatal complications from a chronic disease such as diabetes, or facing a behavioral health crisis that led to suicide or drug overdose.
“All three of those categories could have contributed to an increase in deaths among people who did not have COVID-19 but whose lives were essentially taken by the pandemic,” said Woolf, a professor in the Department of Family Medicine and Population Health at the VCU School of Medicine.
The percentage of excess deaths among non-Hispanic Black individuals (16.9%) exceeded their share of the U.S. population (12.5%), reflecting racial disparities in mortality due to COVID-19 and other causes of death in the pandemic, Woolf and his co-authors write in the paper. The excess death rate among Black Americans was higher than rates of excess deaths among non-Hispanic white or Hispanic populations.
Woolf said his team was motivated to break down this information by race and ethnicity due to mounting evidence that people of color have experienced an increased risk of death from COVID-19.
“We found a disproportionate number of excess deaths among the Black population in the United States,” said Woolf, VCU’s C. Kenneth and Dianne Wright Distinguished Chair in Population Health and Health Equity. “This, of course, is consistent with the evidence about COVID-19 but also indicates that excess deaths from some conditions other than COVID-19 are also occurring at higher rates in the African American population.”
Surges in excess deaths varied across regions of the United States. Northeastern states, such as New York and New Jersey, were among the first hit by the pandemic. Their pandemic curves looked like a capital “A,” Woolf said, peaking in April and returning rapidly to baseline within eight weeks because strict restrictions were put in place. But the increase in excess deaths lasted much longer in other states that lifted restrictions early and were hit hard later in the year. Woolf cited economic or political reasons for decisions by some governors to weakly embrace, or discourage, pandemic control measures such as wearing masks.
“They said they were opening early to rescue the economy. The tragedy is that policy not only cost more lives, but actually hurt their economy by extending the length of the pandemic,” Woolf said. “One of the big lessons our nation must learn from COVID-19 is that our health and our economy are tied together. You can’t really rescue one without the other.”
According to the study’s data, the 10 states with the highest per capita rate of excess deaths were Mississippi, New Jersey, New York, Arizona, Alabama, Louisiana, South Dakota, New Mexico, North Dakota and Ohio.
Nationally, Woolf expects the U.S. will see consequences of the pandemic long after this year. For example, cancer mortality rates may increase in the coming years if the pandemic forced people to delay screening or chemotherapy.
Woolf said future illness and deaths from the downstream consequences of the devastated economy could be addressed now by “bringing help to families, expanding access to health care, improving behavioral health services and trying to bring economic stability to a large part of the population that was already living on the edge before the pandemic.” Among other research, his team’s 2019 JAMA study of working-age mortality underscores the importance of prioritizing public health measures like these, he said.
“American workers are sicker and dying earlier than workers in businesses in other countries that are competing against America,” Woolf said. “So investments to help with health are important for the U.S. economy in that context just as they are with COVID-19.”
Derek Chapman, Ph.D., Roy Sabo, Ph.D., and Emily Zimmerman, Ph.D., of VCU’s Center on Society and Health and the School of Medicine joined Woolf as co-authors on the paper published Friday, “Excess Deaths From COVID-19 and Other Causes in the United States, March 1, 2020, to January 2, 2021.”
Their study also confirms a trend Woolf’s team noted in an earlier 2020 study: Death rates from several non-COVID-19 conditions, such as heart disease, Alzheimer’s disease, and diabetes, increased during surges.
“This country has experienced profound loss of life due to the pandemic and its consequences, especially in communities of color,” said Peter Buckley, M.D., dean of the VCU School of Medicine. “While we must remain vigilant with social distancing and mask-wearing behaviors for the duration of this pandemic, we must also make efforts to ensure the equitable distribution of care if we are to reduce the likelihood of further loss of life.”
Based on current trends, Woolf said the surges the U.S. has seen might not be over, even with vaccinations underway.
“We’re not out of the woods yet because we’re in a race with the COVID-19 variants. If we let up too soon and don’t maintain public health restrictions, the vaccine may not win out over the variants,” Woolf said. “Unfortunately, what we’re seeing is that many states have not learned the lesson of 2020. Once again, they are lifting restrictions, opening businesses back up, and now seeing the COVID-19 variants spread through their population.
“To prevent more excess deaths, we need to hold our horses and maintain the public health restrictions that we have in place so the vaccine can do its work and get the case numbers under control.”
U.S. deaths normally change less than 2% each year. In 2020, they rose nearly 23%.
Suicides Drop During Past Year of Pandemic, Study Finds
By Mark Moran
20 May 2021
(Psychiatric News) – Deaths by suicide declined by almost 6% from 2019 to 2020, according to a report in JAMA based on data from the Centers for Disease Control and Prevention (CDC) [Excess Deaths From COVID-19 and Other Causes in the US, March 1, 2020, to January 2, 2021].
The decline is good news in an otherwise grim report that revealed a 17.7% increase in overall deaths in 2020, with most of those directly attributable to COVID-19.
Importantly, the decrease in the total number of suicide deaths could possibly mask increases among subgroups that have been disproportionately affected by the pandemic. “We do not yet have the data to consider suicide in specific populations based on demographic factors such as age, gender, and racial/ethnic background or social determinants such as income, access to health care, and stressors that minoritized communities may experience,” Moutier said. “Additionally, we know there can be a time lag in the manifestation of distress even months after the acuity of a traumatic or stressful period is over.”
AFSP President Maria A. Oquendo, M.D., Ph.D., who also is a past APA president, agreed and noted especially the increase documented in a 2019 Pediatrics report on Black adolescents showing that suicide attempts rose by 73% between 1991 and 2017, and injury by attempt rose by 122% (Psychiatric News).
“The data for 2020 are not yet available, but increases in suicide rates among Black youth and other minority populations in the prior few years require attention,” Oquendo told Psychiatric News.
Regarding the overall drop in suicide in 2020, Oquendo said it is not entirely surprising that people are less likely to die by suicide in the wake of a collective, community trauma.
“Suicidologists have long observed that suicide rates tend to decline after a catastrophe,” she said. “The reason is unknown, but some hypotheses include the possibility that individuals become more externally focused given the environmental threat, that the community cohesion that sometimes follows catastrophe has beneficent effects, or that community suffering makes personal suffering more tolerable.”
Beyond the encouraging overall decrease in suicide, the JAMA report is a stark portrait of the grim toll the pandemic has taken on the American population. Along with the more than 345,000 known COVID-19 deaths in 2020, increases were also noted for several other leading causes of death.
“These increases may indicate, to some extent, underreporting of COVID-19—that is, limited testing in the beginning of the pandemic may have resulted in underestimation of COVID-19 mortality,” the authors wrote. “Increases in other leading causes, especially heart disease, Alzheimer disease, and diabetes, may also reflect disruptions in health care that hampered early detection and disease management. Increases in unintentional injury deaths in 2020 were largely driven by drug overdose deaths. Final mortality data will help determine the effect of the pandemic on concurrent trends in drug overdose deaths.”
They added: “The effects of the pandemic are likely to continue through 2021 as well because COVID-19 has already caused more than 100,000 deaths this year. However, the effects of COVID-19 on mortality trends may be mitigated in 2021 given better detection and treatment options as well as increasing natural and vaccine-related immunity.” [more]