Covid: Serious failures in WHO and global response, report finds – “It is due to a myriad of failures, gaps, and delays in preparedness and response”
12 May (BBC News) – The Covid-19 pandemic was preventable, an independent review panel has said.
The panel, set up by the World Health Organization, said the combined response of the WHO and global governments was a “toxic cocktail”.
The WHO should have declared a global emergency earlier than it did, its report said, adding that without urgent change the world was vulnerable to another major disease outbreak.
More than 3.3 million people around the world have now died of Covid.
While the US and Europe are beginning to ease restrictions and resume some aspects of pre-pandemic life, the virus is still devastating parts of Asia.
India in particular is seeing record-breaking numbers of new cases and deaths, with severe oxygen shortages in hospitals across the country.
Countries neighbouring India, such as Nepal, are also seeing surges of the virus.
What did the report say?
Covid-19: Make it the Last Pandemic, was compiled by the Independent Panel for Pandemic Preparedness and Response.
Its aim was to find answers as to how the virus had killed more than 3.3 million people and infected more than 159 million.
“The situation we find ourselves in today could have been prevented,” co-chair Ellen Johnson Sirleaf, a former president of Liberia, told reporters.
“It is due to a myriad of failures, gaps and delays in preparedness and response.” [more]
Covid: Serious failures in WHO and global response, report finds
COVID-19: Make it the Last Pandemic
The devastating reality of the COVID-19 pandemic
12 May 2012 (The Independent Panel for Pandemic Preparedness and Response) – COVID-19 has shown how an infectious disease can sweep the globe in weeks and, in the space of a few months, set back sustainable development by years.
By all measures, the impact of the pandemic is massive:
- 148 million people were confirmed infected and more than
- 3 million have died in 223 countries, territories, and areas (as of 28 April 2021);
- at least 17 000 health workers died from COVID-19 during the pandemic’s first year;
- US$ 10 trillion of output is expected to be lost by the end of 2021, and US$ 22 trillion in the period 2020–2025 — the deepest shock to the global economy since the Second World War and the largest simultaneous contraction of national economies since the Great Depression of 1930–32;
- At its highest point in 2020, 90% of schoolchildren were unable to attend school;
- 10 million more girls are at risk of early marriage because of the pandemic;
- gender-based violence support services have seen fivefold increases in demand;
- 115–125 million people have been pushed into extreme poverty.
The language of health statistics and economics cannot convey the depth of disruption as COVID-19 has overturned people’s lives. People are grieving the loss of their loved ones, and those with long-term health impacts from the disease continue to suffer. There are instances where people with cancer have been unable to attend chemotherapy sessions, and people with suspected tuberculosis have not been diagnosed or treated. Market sellers have been unable to work and put food on the table. Women have found their double workload tripled or quadrupled, as they try to maintain the family income, care for the elderly and sick, become teachers for their home-schooled children, and maintain the well-being of their families.
Most dispiriting is that those who had least before the pandemic have even less now. The experience of previous epidemics shows that income inequality increased in affected countries over the five years following each event. Those working in the informal sector have had little or no support. Migrants, refugees, and displaced people have often been shut out of testing services and health facilities. Perhaps 11 million of the poorest girls in the world may never go back to the classroom (8). People living in the poorest countries are at the tail-end of the vaccine queue.
It does not have to be this way.
A groundswell of opinion is determined to address inequality so that we can come out of the pandemic looking forward to a better world, sustaining and expanding responses where they have shown a better path. Governments have offered income support to millions of people in places where, before the pandemic, that had been considered a political impossibility. Campaign-based health services, like immunization, have bounced back rapidly. Service delivery in health is being changed for the better through people-centred initiatives, such as those in telemedicine or with the multi-month dispensing of medications. The links between green and sustainable futures and a pandemic-free world are being drawn more clearly than ever before.
Ending this pandemic as quickly as possible goes hand in hand with preparing to avert another one. Paying attention to what went wrong, as well as to what went right, will be invaluable pointers to ways in which the world can get back on track to realise the 2030 Agenda for Sustainable Development.
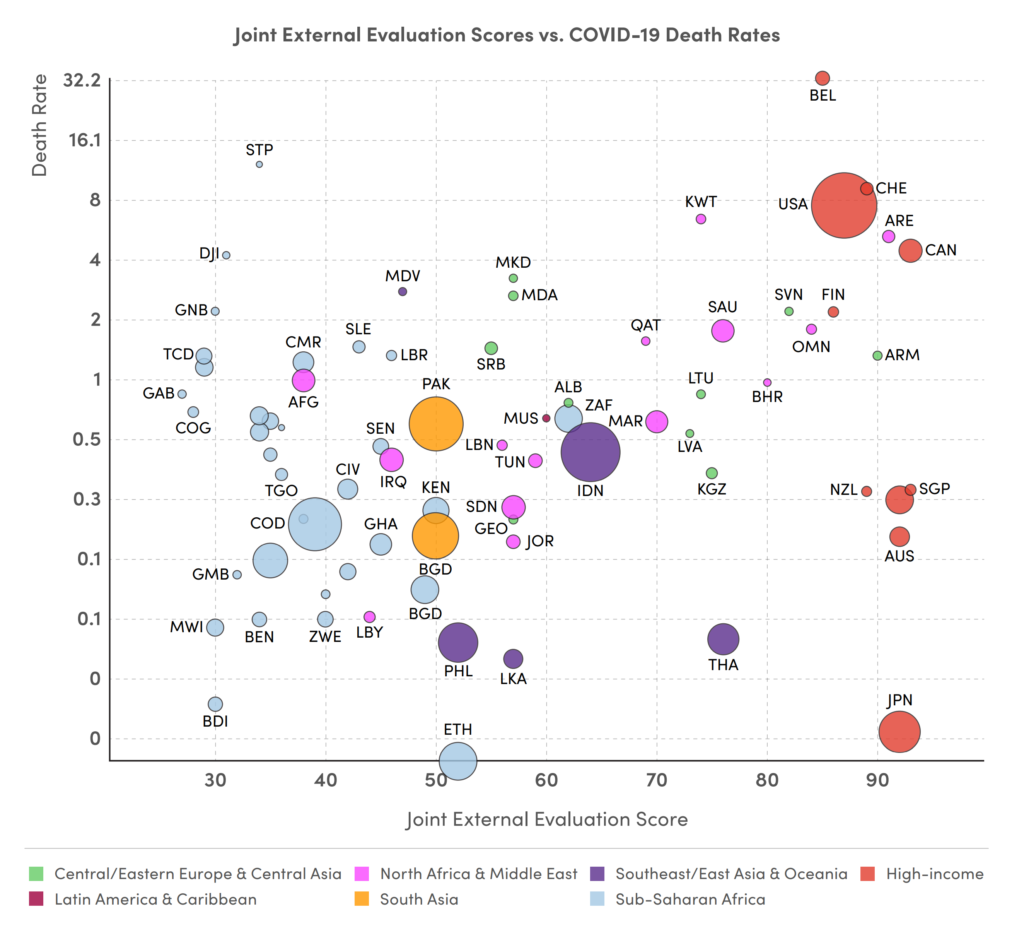
This pandemic has shaken some of the standard assumptions that a country’s wealth will secure its health. Leadership and competence have counted more than cash in pandemic responses. Many of the best examples of decisive leadership have come from governments and communities in more resource-constrained settings. There is a clear opportunity to build a future beyond the pandemic that draws on the wellsprings of wisdom from every part of the world.
The Panel’s call for immediate actions to stop the COVID-19 pandemic
The Panel is deeply concerned and alarmed about the current persistent high levels of transmission of SARSCoV-2, which are driving illness and deaths, and about the development of virus variants all of which continue to impose an intolerable burden on societies and economies.
Countries have varied significantly in their application of public health measures to keep the spread of the virus in check. Some have sought to contain the epidemic aggressively and drive towards elimination; some have aimed at virus suppression; and some have aimed just to mitigate the worst impacts. Countries with the ambition to aggressively contain and stop the spread whenever and wherever it occurs have shown that this is possible. Given what is known already, all countries should apply public health measures consistently and at the scale the epidemiological situation requires. Vaccination alone will not end this pandemic. It must be combined with testing, contact-tracing, isolation, quarantine, masking, physical distancing, hand hygiene, and effective communication with the public.
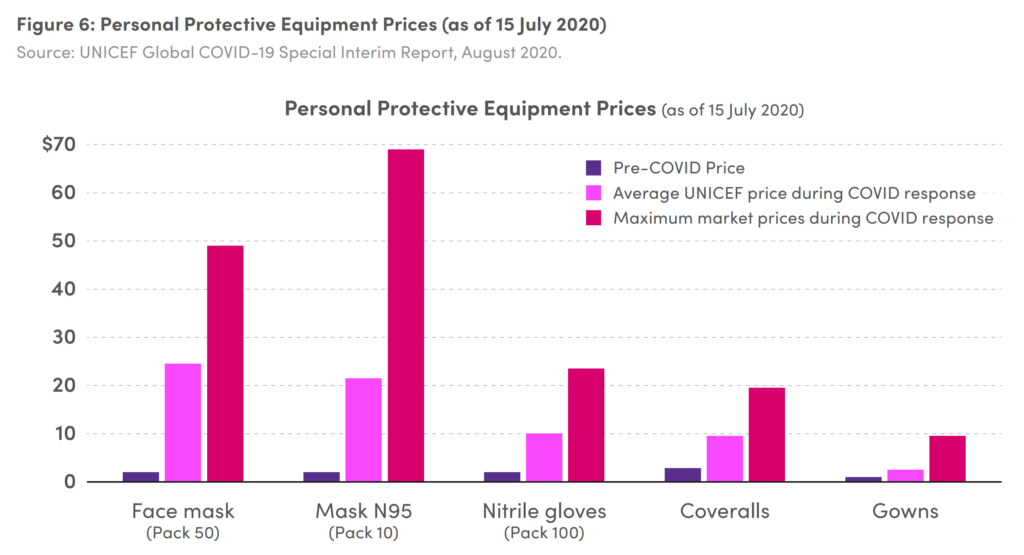
Alongside these non-pharmaceutical measures, vaccine rollout needs to be scaled up urgently and equitably across the world. A number of effective vaccines are now approved. Current production capacity, however, is stretched close to its limits, and vaccination coverage is far from being at the scale needed to reduce the burden of illness and curb transmission globally.
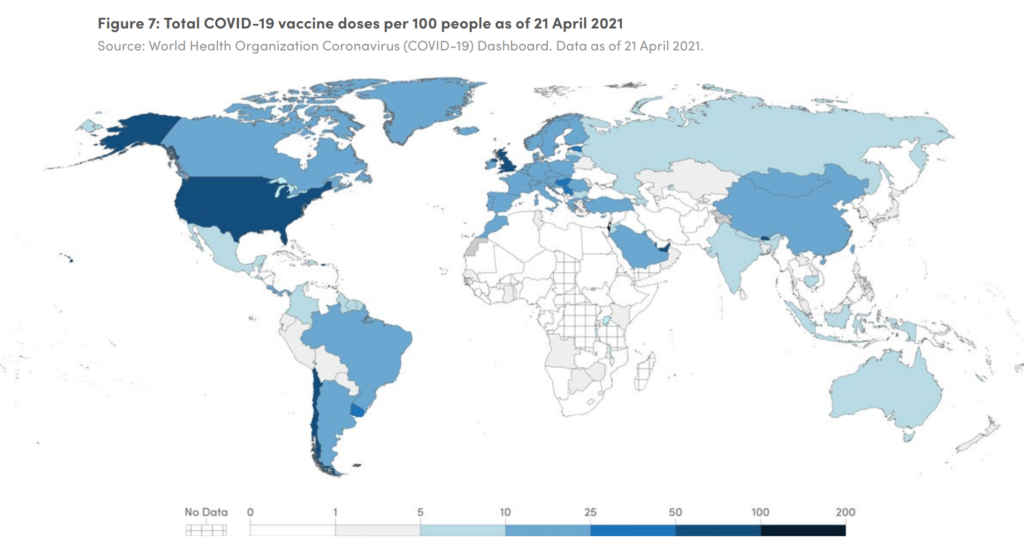
The uneven access to vaccination is one of today’s pre-eminent global challenges. High-income countries have over 200% population coverage of vaccine doses, obtained mainly through bilateral deals with manufacturers to secure existing and future stocks. In many cases low- and middle-income countries have been shut out of these arrangements. In the poorest countries, at the time of finalising this report, fewer than 1% of people have had a single dose of vaccine. The COVID-19 Vaccines Global Access Facility (COVAX Facility), rapidly established with the intention of ensuring global, equitable access, is making good progress but has been hampered in that goal by a lack of sufficient funds and by vaccine nationalism, and now, vaccine diplomacy.
There are 5.7 billion people in the world aged 16 and over. All need access to safe and effective COVID-19 vaccines.
This is not some aspiration for tomorrow — it is urgent, now.
To prepare ourselves for new phases of the COVID-19 pandemic and to respond effectively, a global strategy with clear goals, milestones and priority actions is needed. The significant inequity in vaccine access must be addressed immediately, as it is not only unjust, but also threatens the effectiveness of global efforts to control the pandemic. Variants may still emerge that our vaccines cannot manage. The more quickly we vaccinate now, the less likelihood there is of ever more variants emerging. One action which can be taken now is an equitable redistribution of available vaccine doses. Scaling up the development and supply of therapeutics and of diagnostic tests is also very urgent to save lives.
Moreover, to prepare for likelihood of of COVID-19 becoming endemic and to address inequity in vaccine access in a more sustained way, manufacturing capacity of mRNA and other vaccines must urgently be built in Africa, Latin America and other low- and middle-income regions. Vaccine manufacturing is highly specialized and difficult. Boosting production takes time so enabling it must begin now. It requires agreements on voluntary licensing and technology transfer.
There are 5.7 billion people in the world aged 16 and over. All need access to safe and effective COVID-19 vaccines. This is not some aspiration for tomorrow — it is urgent, now. COVAX has secured 1.1 billion vaccine doses and has optioned 2.5 billion more (9). Before the end of April, one billion vaccine doses were administered, overwhelmingly in high-income or upper-middle-income countries. The Panel joins with political and faith leaders across the world and calls for an all-out effort to reach the world’s population with vaccines within a year and set in place the infrastructure needed for at least 5 billion booster doses annually.
Immediate action to end COVID-19 must be guided by explicit strategies with measurable milestones. The Panel recognizes the WHO COVID-19 Strategic Preparedness and Response Plan for 2021 (10) provides useful technical guidance but the Panel’s view is that there is a need for a higher level roadmap for ending the pandemic with clear targets, milestones, and dates.
The Independent Panel makes the following urgent calls
I. Apply non-pharmaceutical public health measures systematically and rigorously in every country at the scale the epidemiological situation requires. All countries to have an explicit evidence-based strategy agreed at the highest level of government to curb COVID-19 transmission.
II. High-income countries with a vaccine pipeline for adequate coverage should, alongside their scale-up, commit to provide to the 92 low and middle-income countries of the Gavi COVAX Advance Market Commitment, at least one billion vaccine doses no later than 1 September 2021 and more than two billion doses by mid-2022, to be made available through COVAX and other coordinated mechanisms.
III. G7 countries to commit to providing 60% of the US$ 19 billion required for ACT-A in 2021 for vaccines, diagnostics, therapeutics and strengthening health systems with the remainder being mobilised from others in the G20 and other higher income countries. A formula based on ability to pay should be adopted for predictable, sustainable, and equitable financing of such global public goods on an ongoing basis.
IV. The World Trade Organization and WHO to convene major vaccine-producing countries and manufacturers to get agreement on voluntary licensing and technology transfer arrangements for COVID-19 vaccines (including through the Medicines Patent Pool). If actions do not occur within three months, a waiver of intellectual property rights under the Agreement on Trade-Related Aspects of Intellectual Property Rights should come into force immediately.
V. Production of and access to COVID-19 tests and therapeutics, including oxygen, should be scaled up urgently in low- and middle-income countries with full funding of US$1.7 billion for needs in 2021 and the full utilization of the US$3.7 billion in the Global Fund’s COVID-19 Response Mechanism Phase 2 for procuring tests, strengthening laboratories and running surveillance and tests.
VI. WHO to develop immediately a roadmap for the short-term, and within three months scenarios for the medium- and long-term response to COVID-19, with clear goals, targets, and milestones to guide and monitor the implementation of country and global efforts towards ending the COVID-19 pandemic. [more]