UK after Brexit: “Shocking” emergency room delays “killing up to 500 people a week” as NHS care collapses – “We are seeing equivalent levels of pressure to the early months of Covid”
By Rhys Blakely and Henry Zeffman
2 January 2023
(The Times) – As many as 500 people are dying each week because of delays in emergency NHS care, a senior doctor has said.
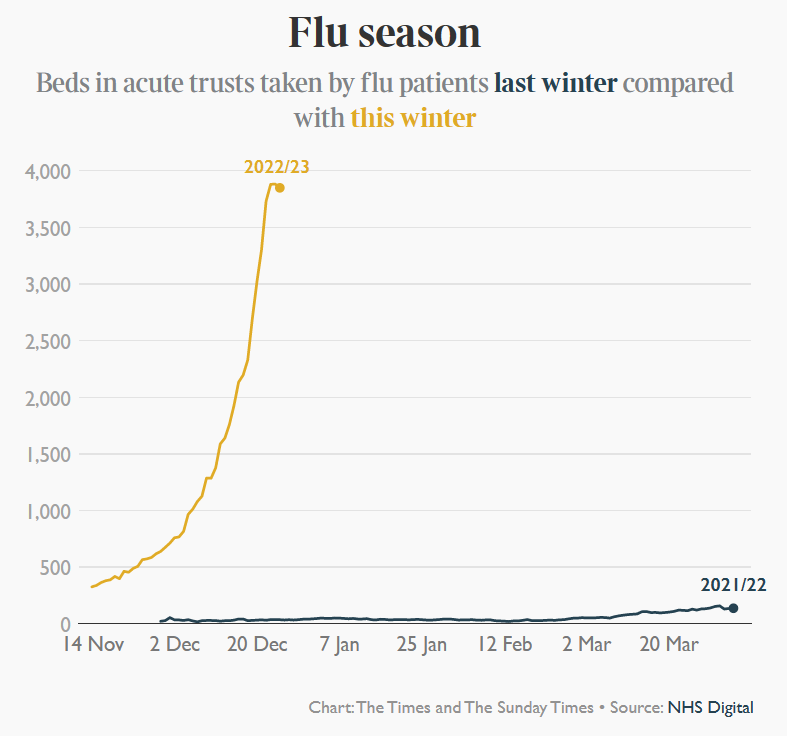
Dr Adrian Boyle, president of the Royal College of Emergency Medicine (RCEM), said that a bad flu season was piling pressure on to services that were already critically overstretched.
A collapse in ambulance response times, gridlock in A&E units and soaring rates of staff turnover were contributing to avoidable deaths, he said.
“We think somewhere between 300 and 500 people are dying as a consequence of delays and problems with urgent and emergency care each week,” he told Times Radio.
The comments will magnify concerns about the state of the health service as thousands more paramedics, nurses and doctors prepare to walk out over pay and conditions. A healthcare leader said yesterday that hospitals were under as much pressure as at the start of the pandemic, while a senior medic urged the government to declare a national major incident.
Ambulance staff are due to strike on January 11 and 23, while nurses will walk out on January 18 and 19. A ballot for industrial action by junior doctors in England will open on January 9.
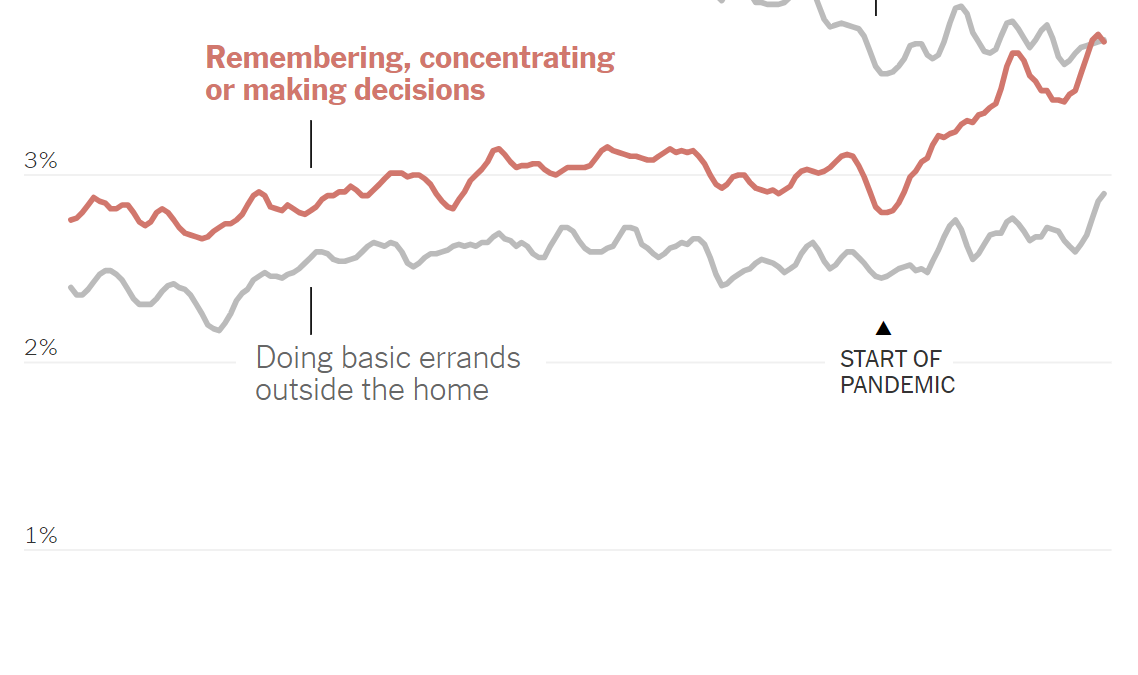
While ministers hope that continuing industrial action will erode public support for the strikers, a crisis in emergency care could also rebound on the government. Health leaders are already confronting a rise in excess deaths, with Sir Chris Whitty warning that Britain faces a “prolonged period” of high death rates because people stayed away from the NHS during the pandemic or could not get treatment.
Whitty, the chief medical officer for England, has warned ministers that thousands of middle-aged people are dying of heart conditions because they did not get statins or blood pressure medicines in 2020 and 2021.
Hundreds more people a week are dying than normal, with the reasons not fully understood. Ambulance delays have also been cited by senior doctors as worsening the death toll.

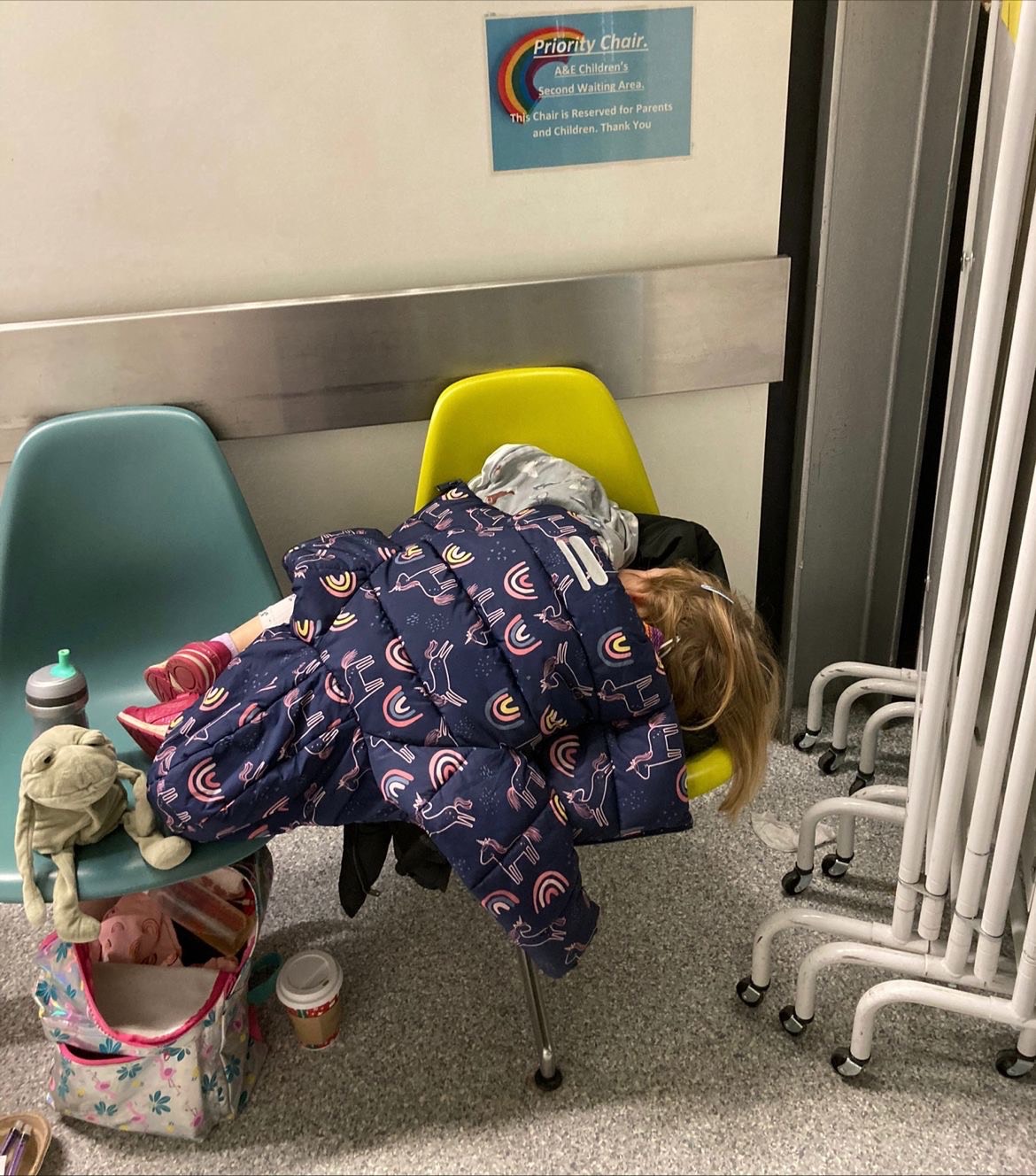
Hit by a flu and Covid “twindemic”, dozens of hospital trusts have declared critical incidents, with record numbers of patients being treated in corridors and some departments running short of portable oxygen cylinders. The longest wait for a bed is thought to have been at Great Western Hospital, Swindon, where a patient spent 99 hours last week before a place could be found on a ward, The Sunday Times reported.
Saffron Cordery, the interim chief executive of NHS Providers, which represents hospital trusts, said: “I think we are seeing equivalent levels of pressure [to the early months of Covid].”
Dr Tim Cooksley, president of the Society for Acute Medicine, called the situation in urgent and emergency care “shocking” and urged the government to declare a national NHS major incident, enabling the four nations to manage demand across the UK. [more]