Drug-resistant bacteria kill 1.2 million globally – “This new study clearly demonstrates the existential threat that resistance poses to global health and modern medicine”
By Mike Stobbe
20 January 2022
NEW YORK (AP) – Antibiotic-resistant germs caused more than 1.2 million deaths globally in one year, according to new research that suggests that these “superbugs” have joined the ranks of the world’s leading infectious disease killers.
The new estimate, published Thursday in the medical journal Lancet, is not a complete count of such deaths, but rather an attempt to fill in gaps from countries that report little or no data on the germs’ toll.
The World Health Organization has been citing a global estimate — several years old — that suggested at least 700,000 people die each year due to antimicrobial-resistant germs. But health officials have long acknowledged that there’s been very little information from many countries.
Antimicrobial resistance happens when germs like bacteria and fungi gain the power to fight off the drugs that were designed to kill them. The problem is not new, but attention to it has grown amid worries about a lack of new drugs to fight the germs.
WHO officials said in a statement that the new study “clearly demonstrates the existential threat” that drug-resistant germs pose.
In the last few decades, health officials have tried to step up efforts to find funding and solutions. That includes trying to get a better handle on the toll. In the U.S., the Centers for Disease Control in 2019 estimated that more than 35,000 Americans die each year from antibiotic-resistant infections — or about 1% of the people who develop such infections.
In the new paper, the researchers estimated deaths linked to 23 germs in 204 countries and territories in 2019. They used data from hospitals, surveillance systems, other studies and other sources to produces death estimates in all parts of the world.
They concluded that more than 1.2 million people died in 2019 from antibiotic-resistant bacterial infections, which are a large subset of a resistance problem also seen in drugs that target fungi and viruses.
The estimate — which includes drug-resistant tuberculosis deaths — suggests the annual toll of such germs is higher than such global scourges as HIV and malaria. [more]
Study: Drug-resistant bacteria kill 1.2 million globally
Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis
ABSTRACT: We estimated deaths and disability-adjusted life-years (DALYs) attributable to and associated with bacterial AMR for 23 pathogens and 88 pathogen–drug combinations in 204 countries and territories in 2019. We obtained data from systematic literature reviews, hospital systems, surveillance systems, and other sources, covering 471 million individual records or isolates and 7585 study-location-years. We used predictive statistical modelling to produce estimates of AMR burden for all locations, including for locations with no data. Our approach can be divided into five broad components: number of deaths where infection played a role, proportion of infectious deaths attributable to a given infectious syndrome, proportion of infectious syndrome deaths attributable to a given pathogen, the percentage of a given pathogen resistant to an antibiotic of interest, and the excess risk of death or duration of an infection associated with this resistance. Using these components, we estimated disease burden based on two counterfactuals: deaths attributable to AMR (based on an alternative scenario in which all drug-resistant infections were replaced by drug-susceptible infections), and deaths associated with AMR (based on an alternative scenario in which all drug-resistant infections were replaced by no infection). We generated 95% uncertainty intervals (UIs) for final estimates as the 25th and 975th ordered values across 1000 posterior draws, and models were cross-validated for out-of-sample predictive validity. We present final estimates aggregated to the global and regional level.
Findings
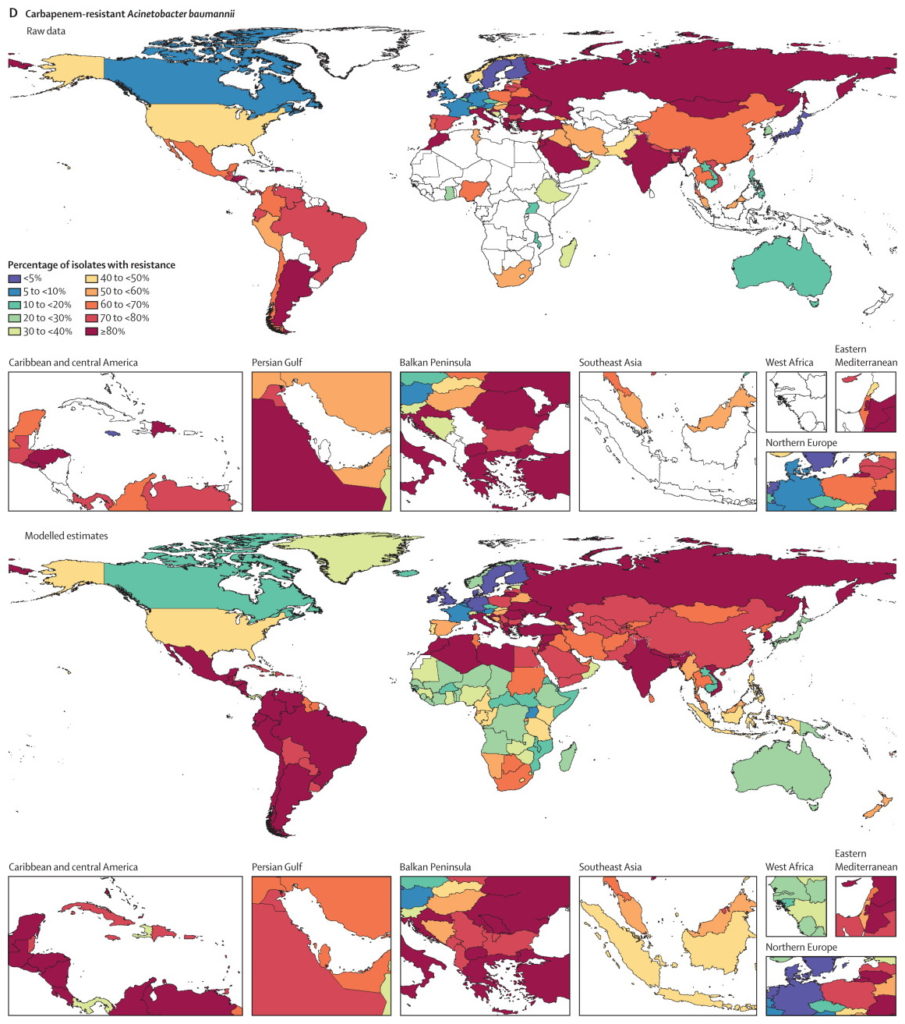
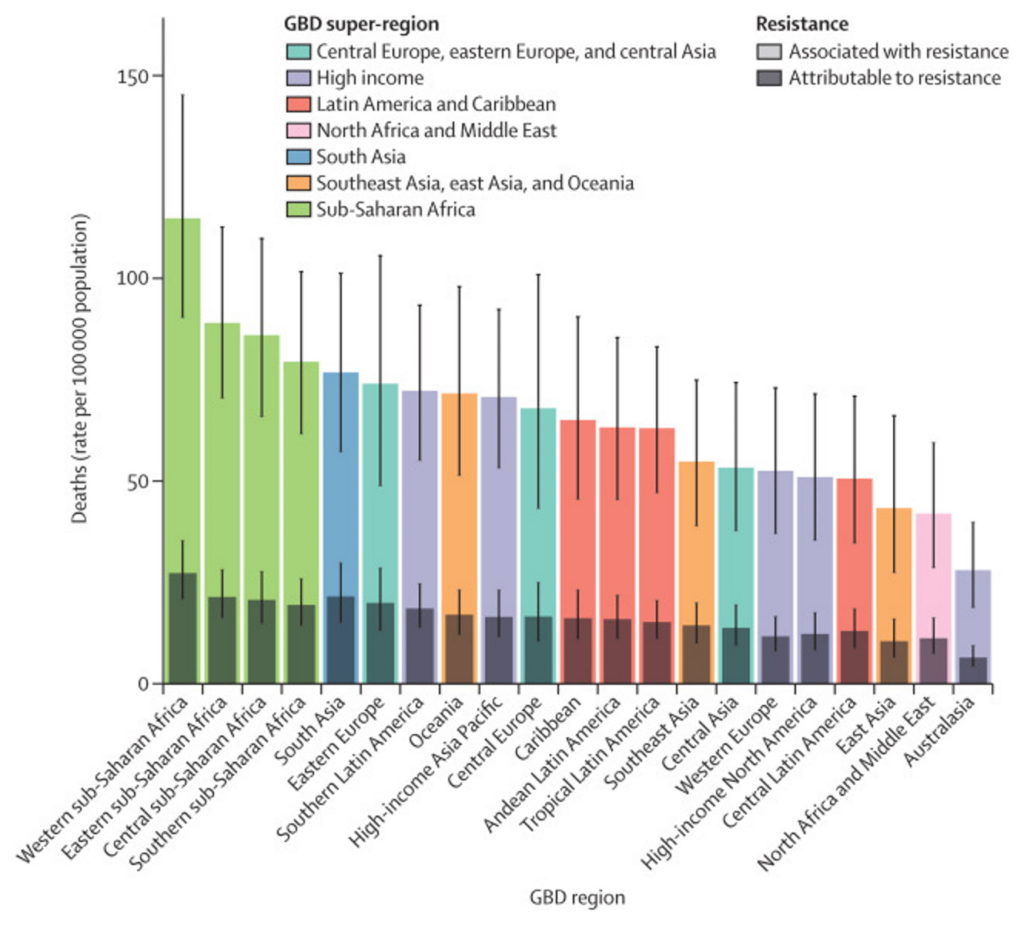
On the basis of our predictive statistical models, there were an estimated 4·95 million (3·62–6·57) deaths associated with bacterial AMR in 2019, including 1·27 million (95% UI 0·911–1·71) deaths attributable to bacterial AMR. At the regional level, we estimated the all-age death rate attributable to resistance to be highest in western sub-Saharan Africa, at 27·3 deaths per 100 000 (20·9–35·3), and lowest in Australasia, at 6·5 deaths (4·3–9·4) per 100 000. Lower respiratory infections accounted for more than 1·5 million deaths associated with resistance in 2019, making it the most burdensome infectious syndrome. The six leading pathogens for deaths associated with resistance (Escherichia coli, followed by Staphylococcus aureus, Klebsiella pneumoniae, Streptococcus pneumoniae, Acinetobacter baumannii, and Pseudomonas aeruginosa) were responsible for 929 000 (660 000–1 270 000) deaths attributable to AMR and 3·57 million (2·62–4·78) deaths associated with AMR in 2019. One pathogen–drug combination, meticillin-resistant S aureus, caused more than 100 000 deaths attributable to AMR in 2019, while six more each caused 50 000–100 000 deaths: multidrug-resistant excluding extensively drug-resistant tuberculosis, third-generation cephalosporin-resistant E coli, carbapenem-resistant A baumannii, fluoroquinolone-resistantE coli, carbapenem-resistant K pneumoniae, and third-generation cephalosporin-resistant K pneumoniae.
Interpretation
To our knowledge, this study provides the first comprehensive assessment of the global burden of AMR, as well as an evaluation of the availability of data. AMR is a leading cause of death around the world, with the highest burdens in low-resource settings. Understanding the burden of AMR and the leading pathogen–drug combinations contributing to it is crucial to making informed and location-specific policy decisions, particularly about infection prevention and control programmes, access to essential antibiotics, and research and development of new vaccines and antibiotics. There are serious data gaps in many low-income settings, emphasising the need to expand microbiology laboratory capacity and data collection systems to improve our understanding of this important human health threat.
Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis